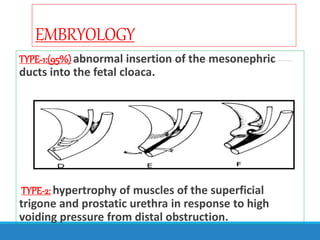
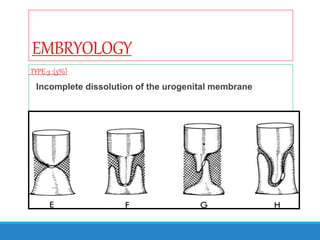
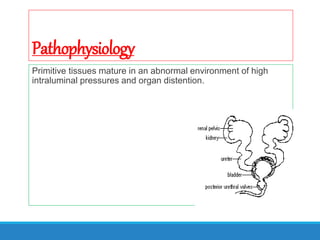
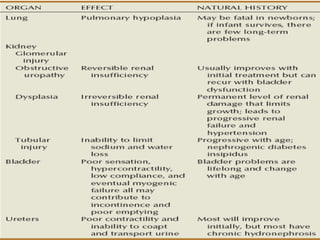
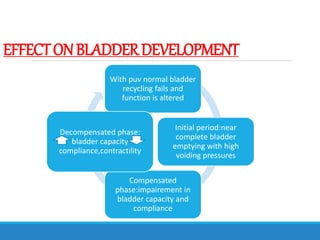
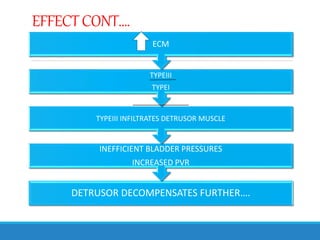
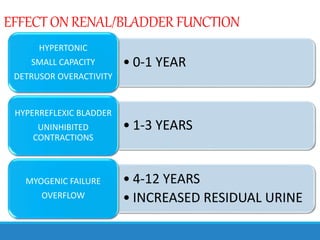
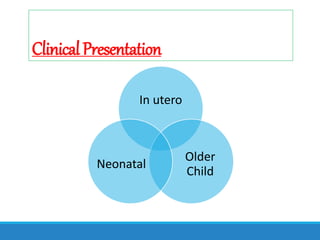
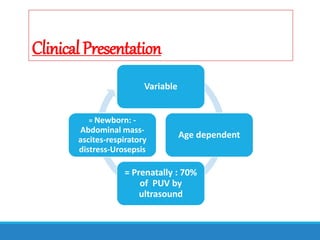
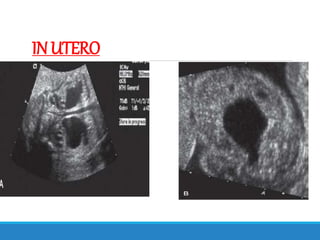
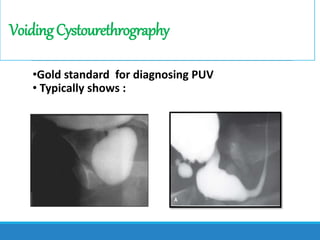
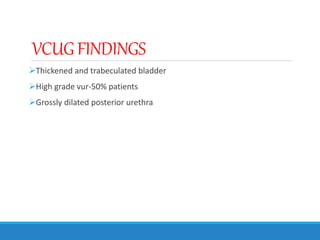
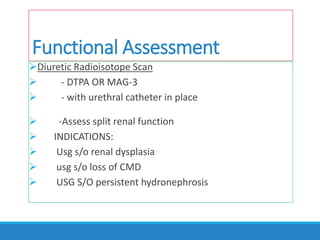
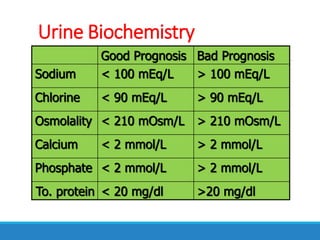
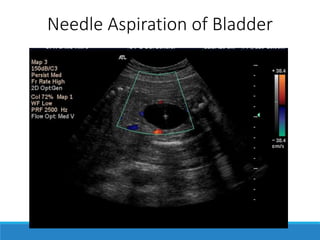
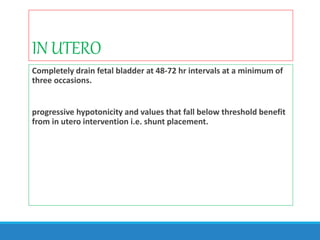
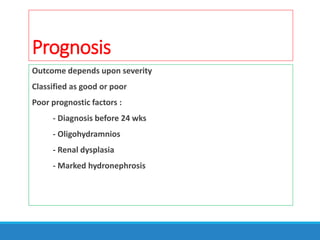
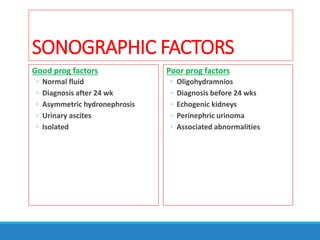
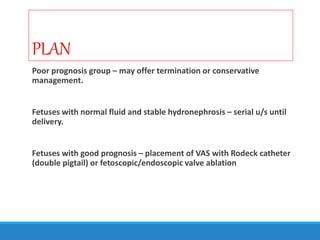
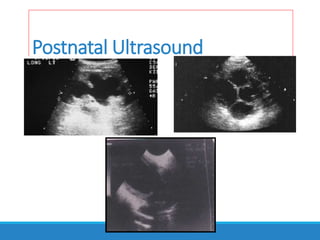
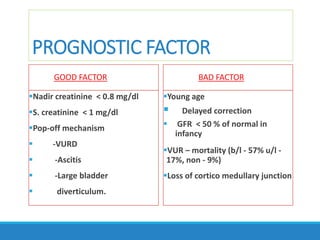
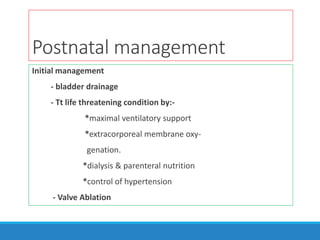
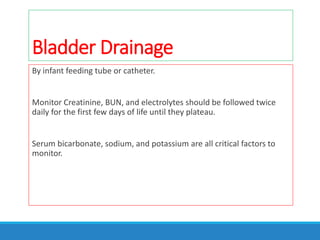
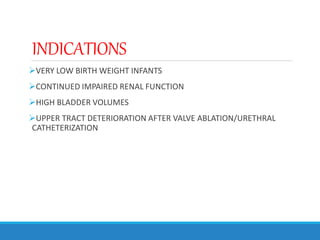
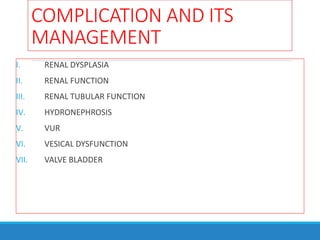
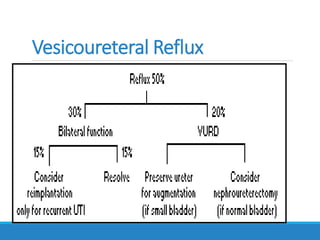
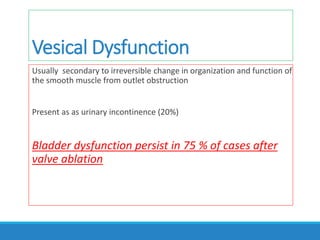
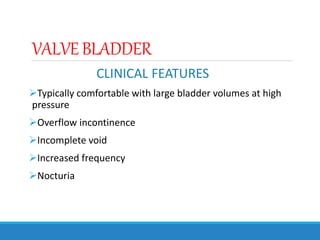
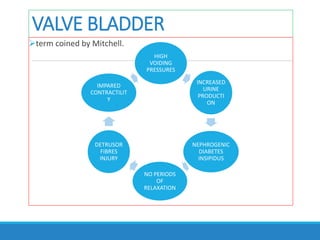
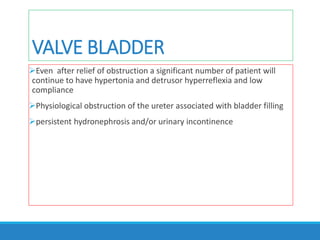
This document provides an overview of the evaluation and management of posterior urethral valves. It begins with an introduction discussing the history and embryology of PUV. It then covers the clinical presentation, diagnostic evaluation, management including in utero and postnatal approaches, complications, and long-term outcomes. Key points include that PUV causes obstructive changes that damage the urinary tract, early diagnosis and relief of obstruction is important to preserve renal function, and bladder dysfunction often persists long-term requiring lifelong management.