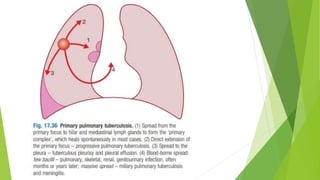
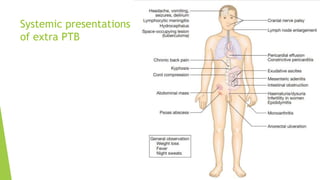
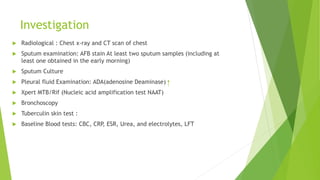
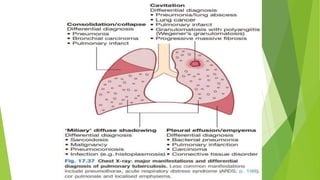
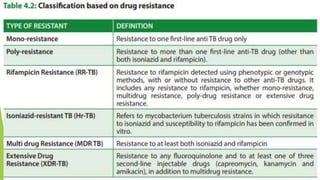
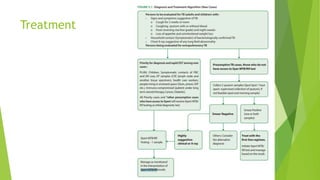
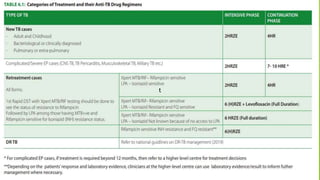
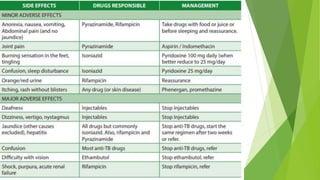
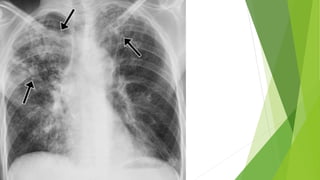
Pulmonary tuberculosis (PTB) is a major communicable disease caused by Mycobacterium tuberculosis, contributing significantly to global mortality. In Nepal, about 42,000 cases were reported in 2018, with higher incidence rates among men and links to several predisposing factors such as age, smoking, and immunosuppression. Diagnosis involves various investigations like sputum examinations and chest radiography, while treatment typically includes a combination of first- and second-line antibiotics, with emphasis on prevention strategies such as vaccination and regular check-ups.