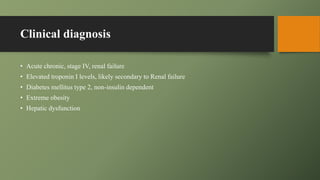
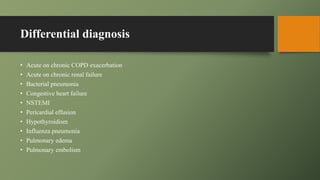
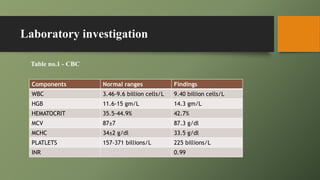
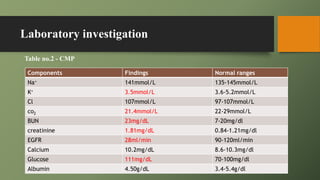
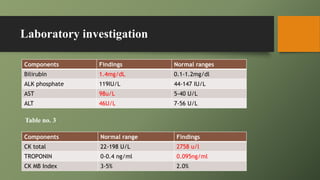
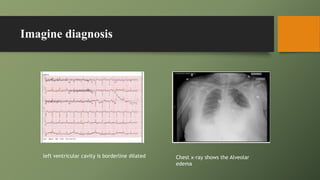
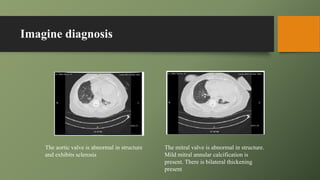
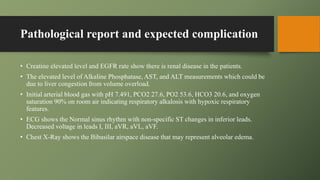
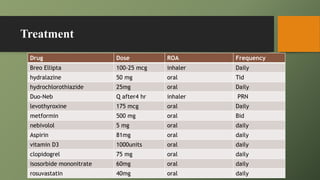
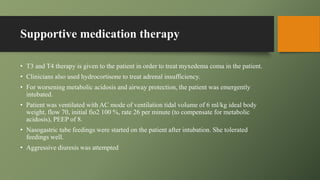
This document presents a case study of a 60-year-old woman experiencing shortness of breath and other symptoms, diagnosed with myxedema coma and acute respiratory failure among other conditions. It details her clinical diagnoses, laboratory findings indicating renal failure and liver congestion, imaging results, and treatment interventions including supportive care. The patient's condition improved with treatment, but challenges with medication compliance were noted, leading to a focus on supportive therapy.