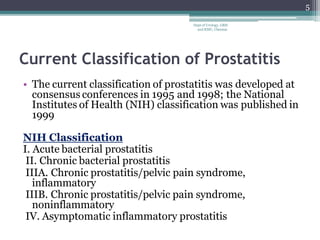
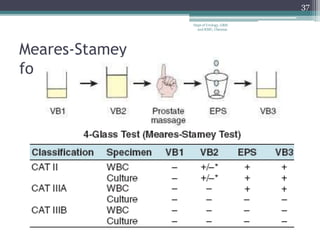
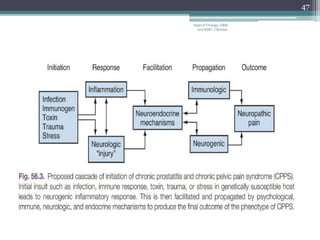
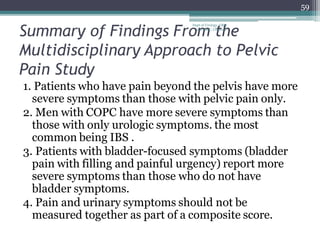
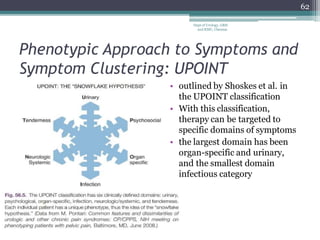
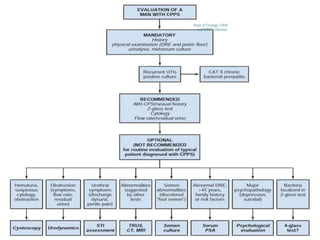
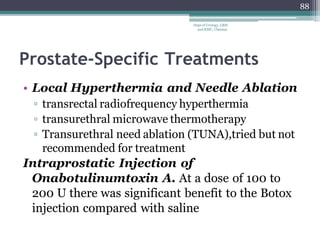
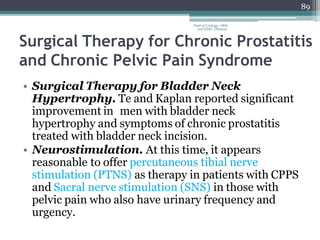
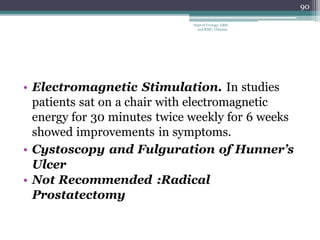
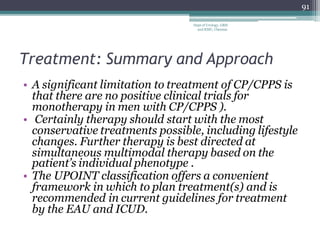
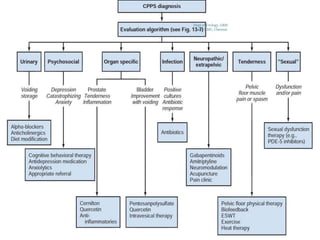
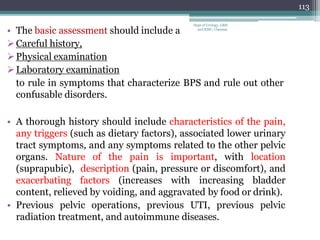
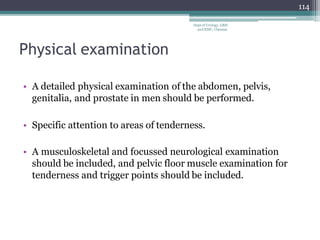
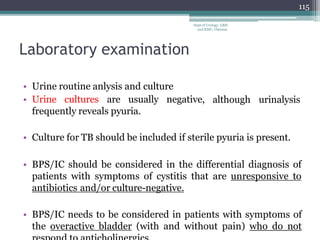
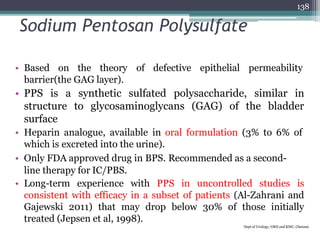
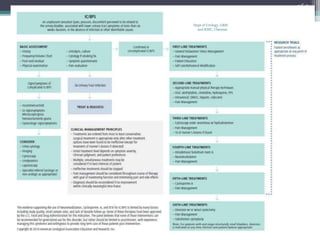
The document discusses the history, classification, diagnosis, and treatment of prostatitis, chronic pelvic pain syndrome, and interstitial cystitis. It details the evolution of prostatitis definitions, histopathology findings, and the current National Institutes of Health (NIH) classification system, which includes categories of prostatitis based on symptoms and microbiological findings. Furthermore, it outlines treatment approaches, which often include antibiotics and patient management strategies tailored to specific types of prostatitis.