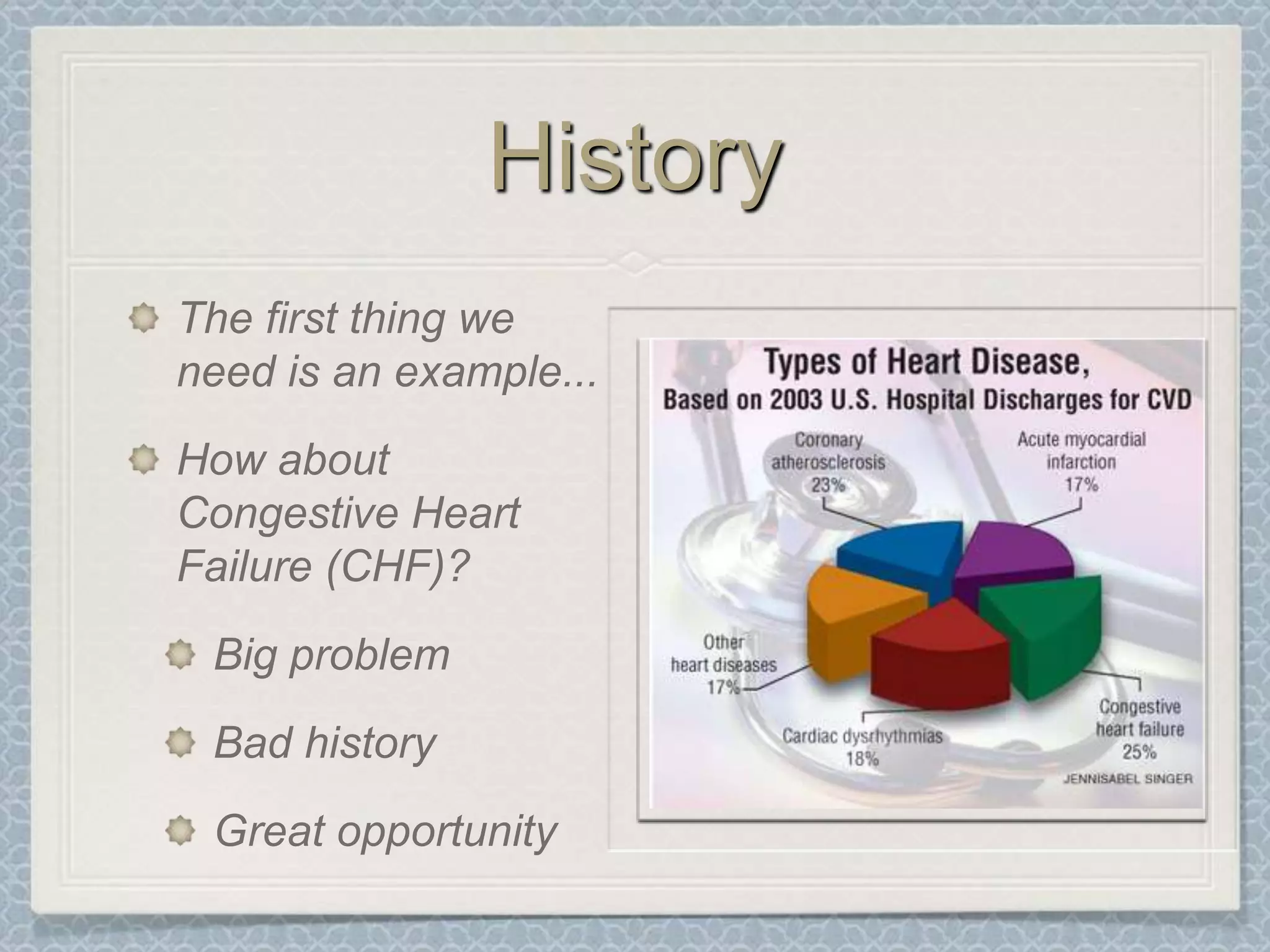
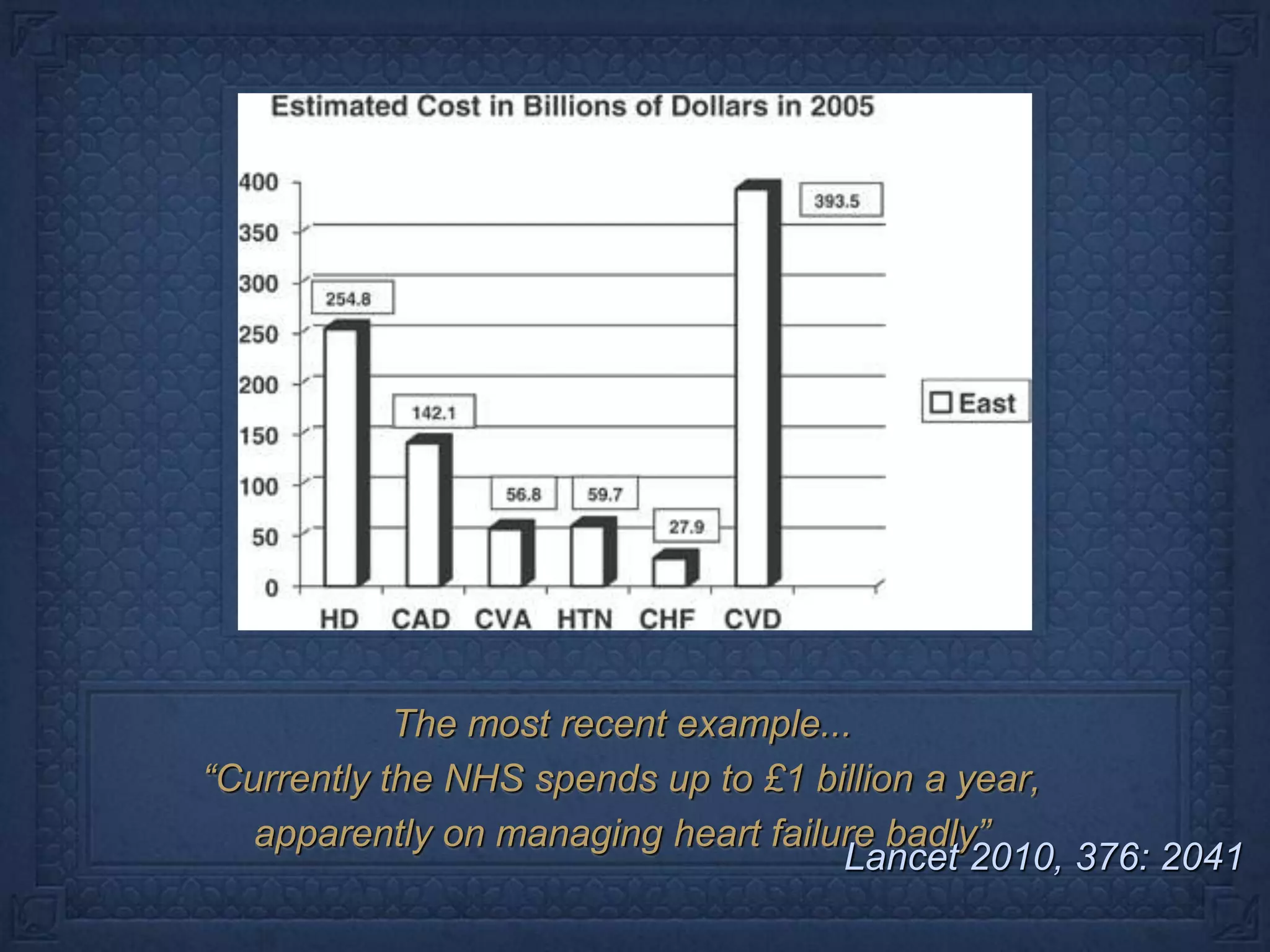
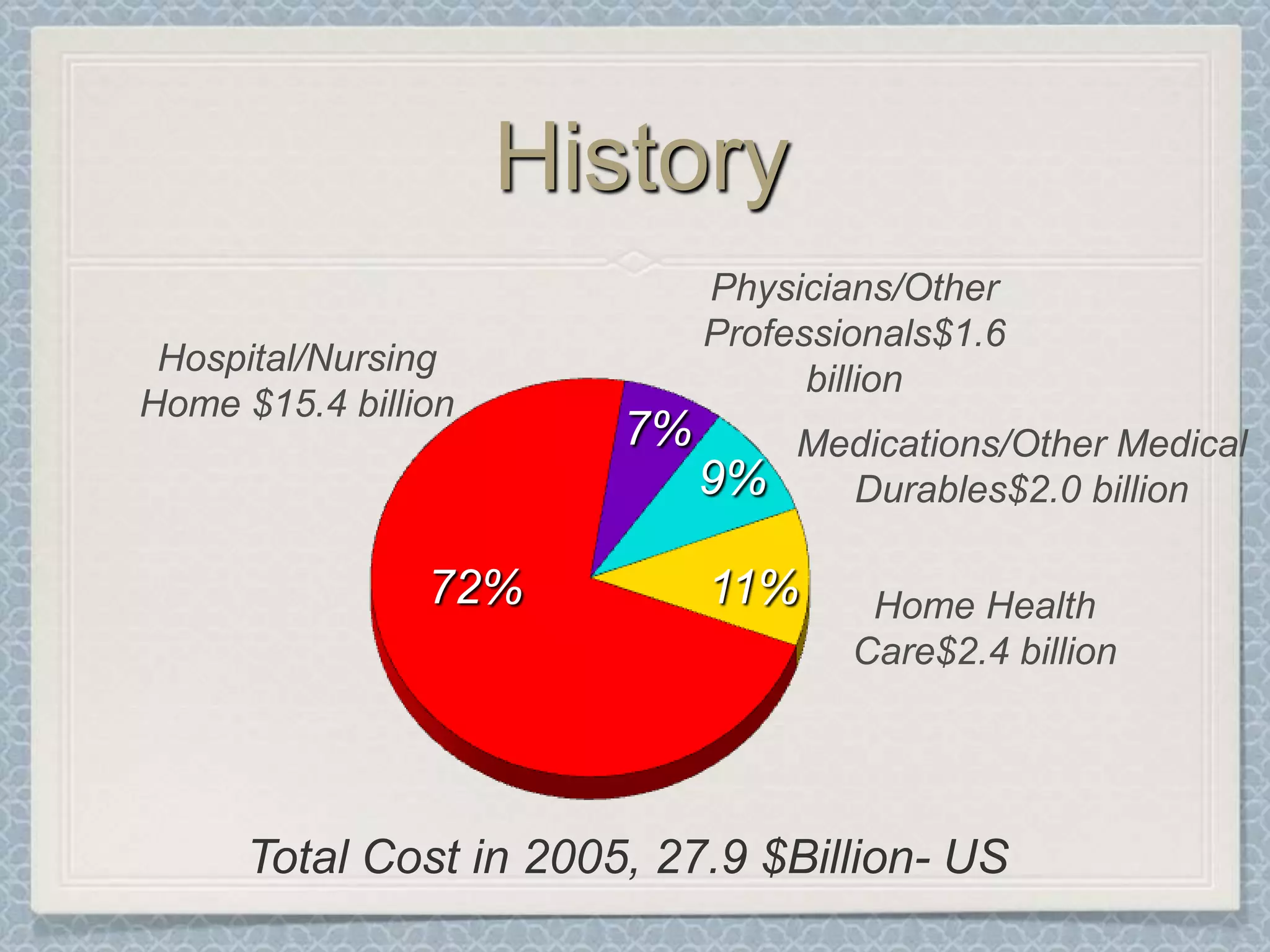
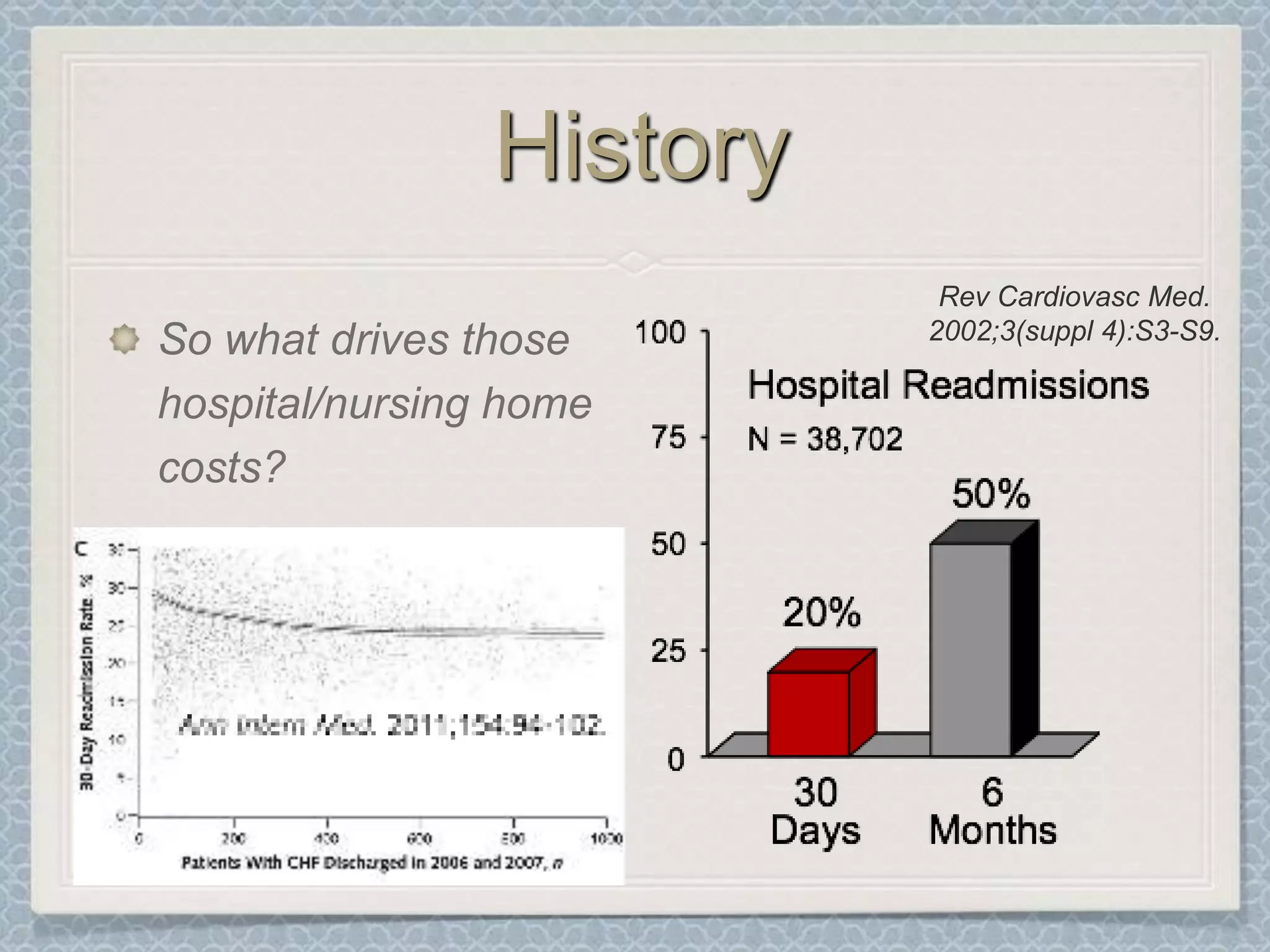
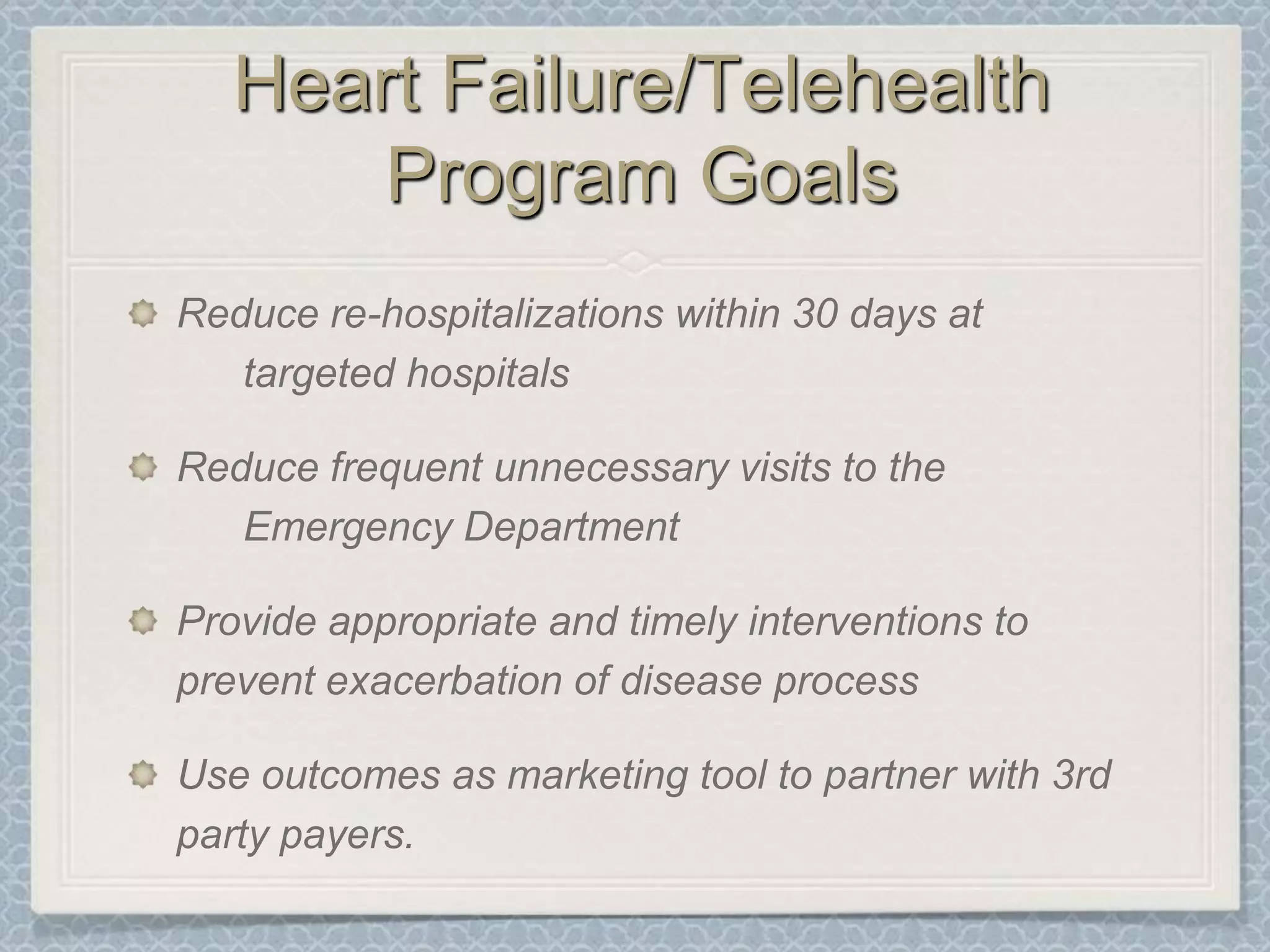
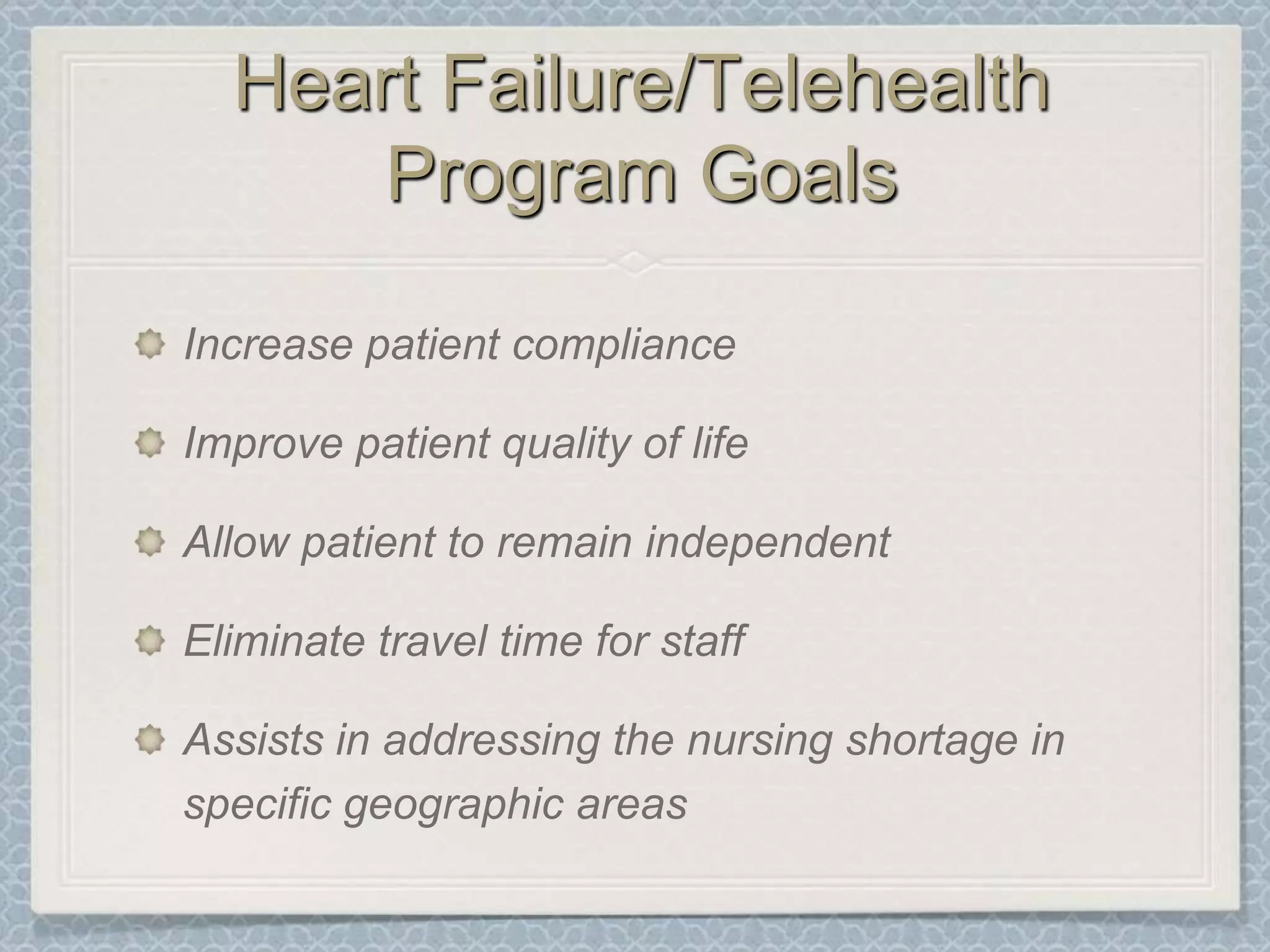
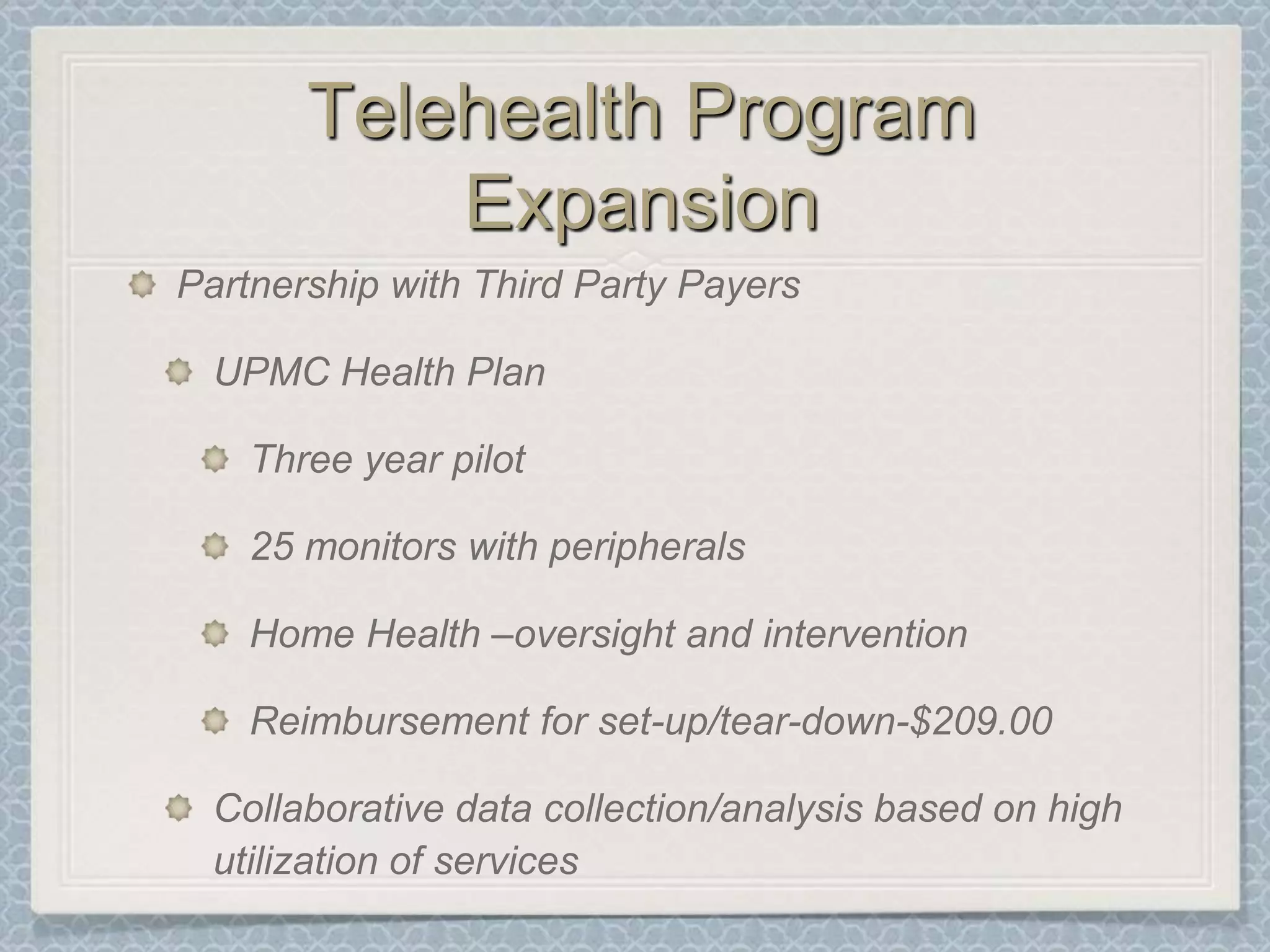
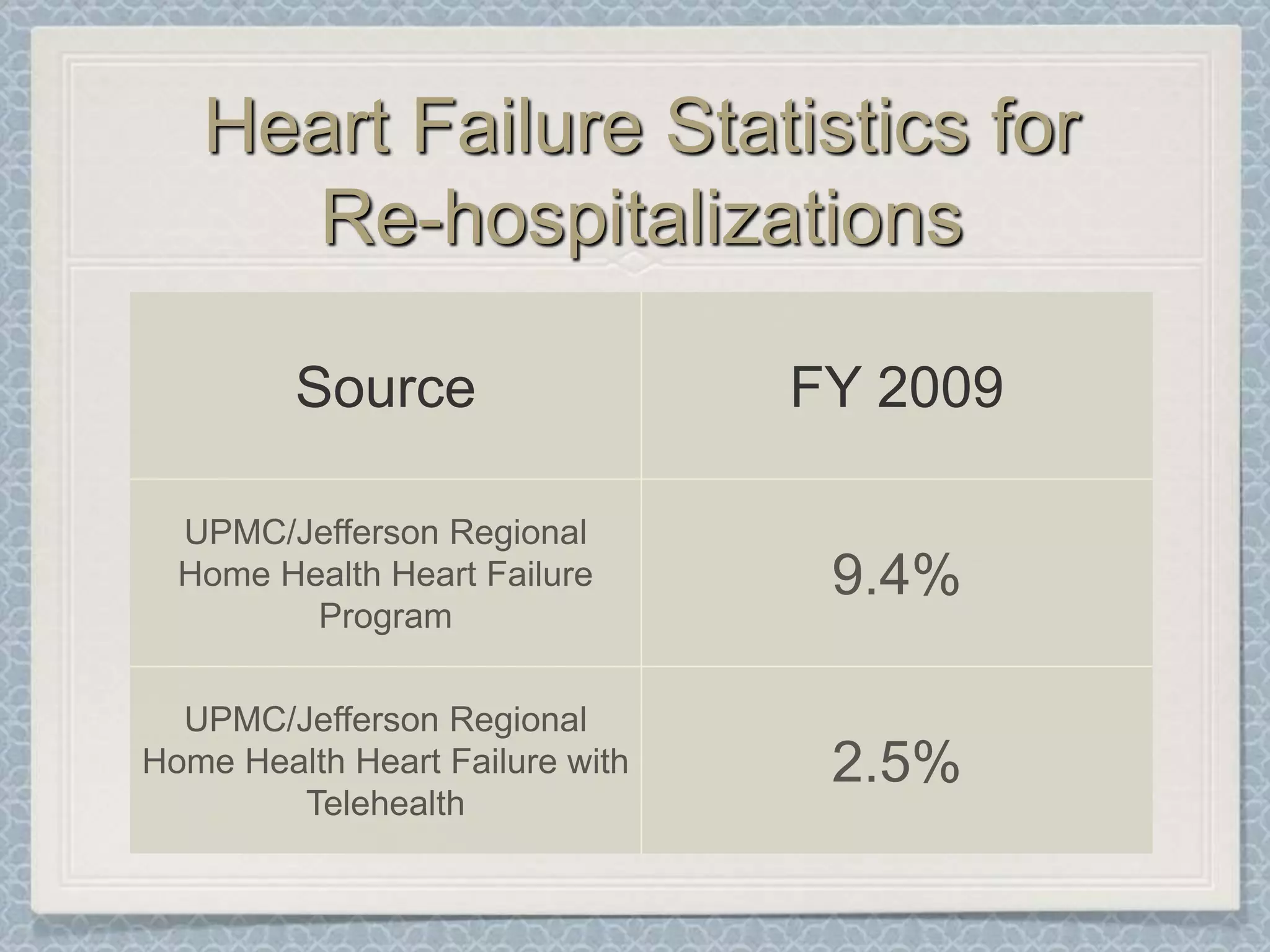
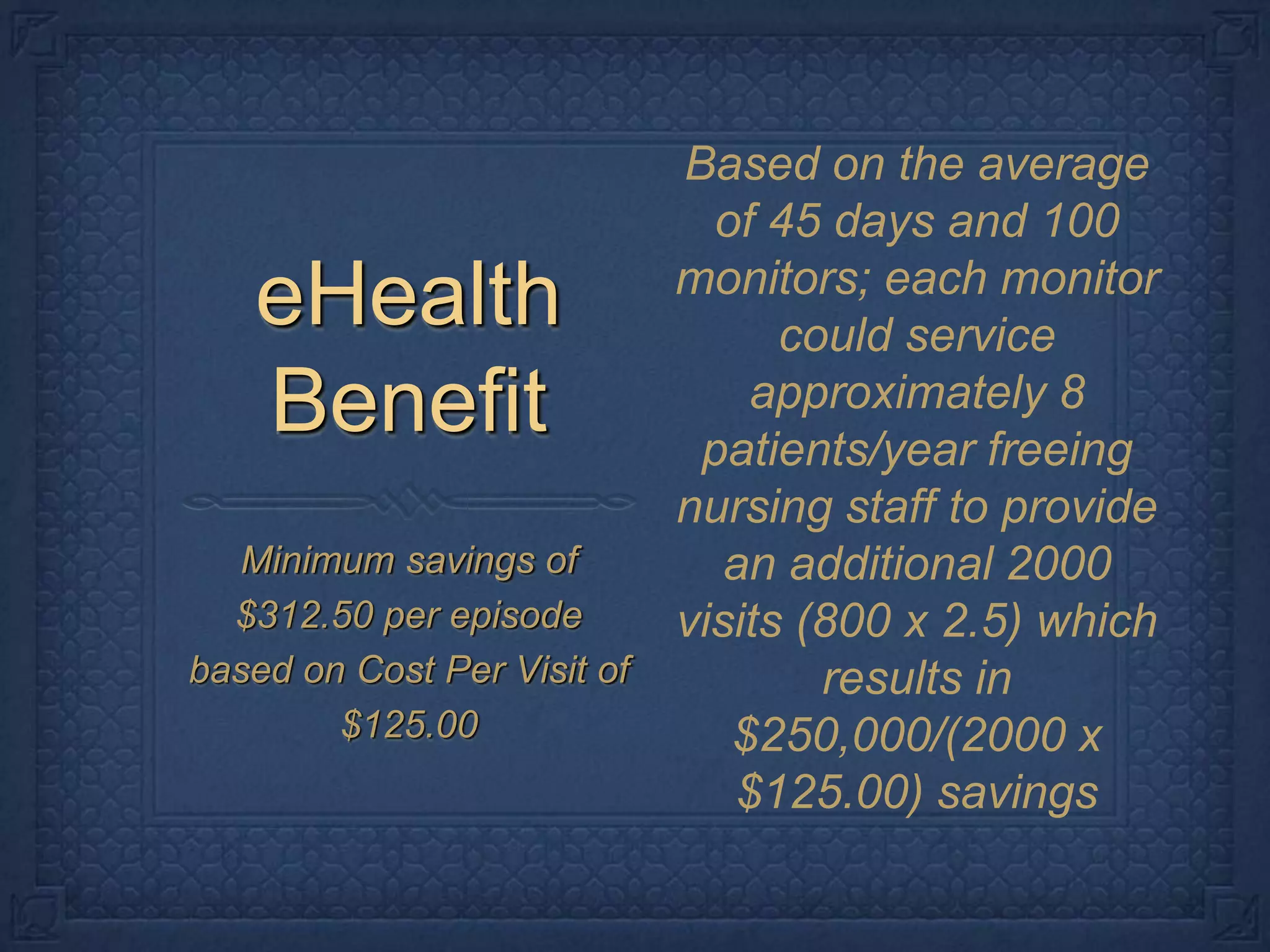
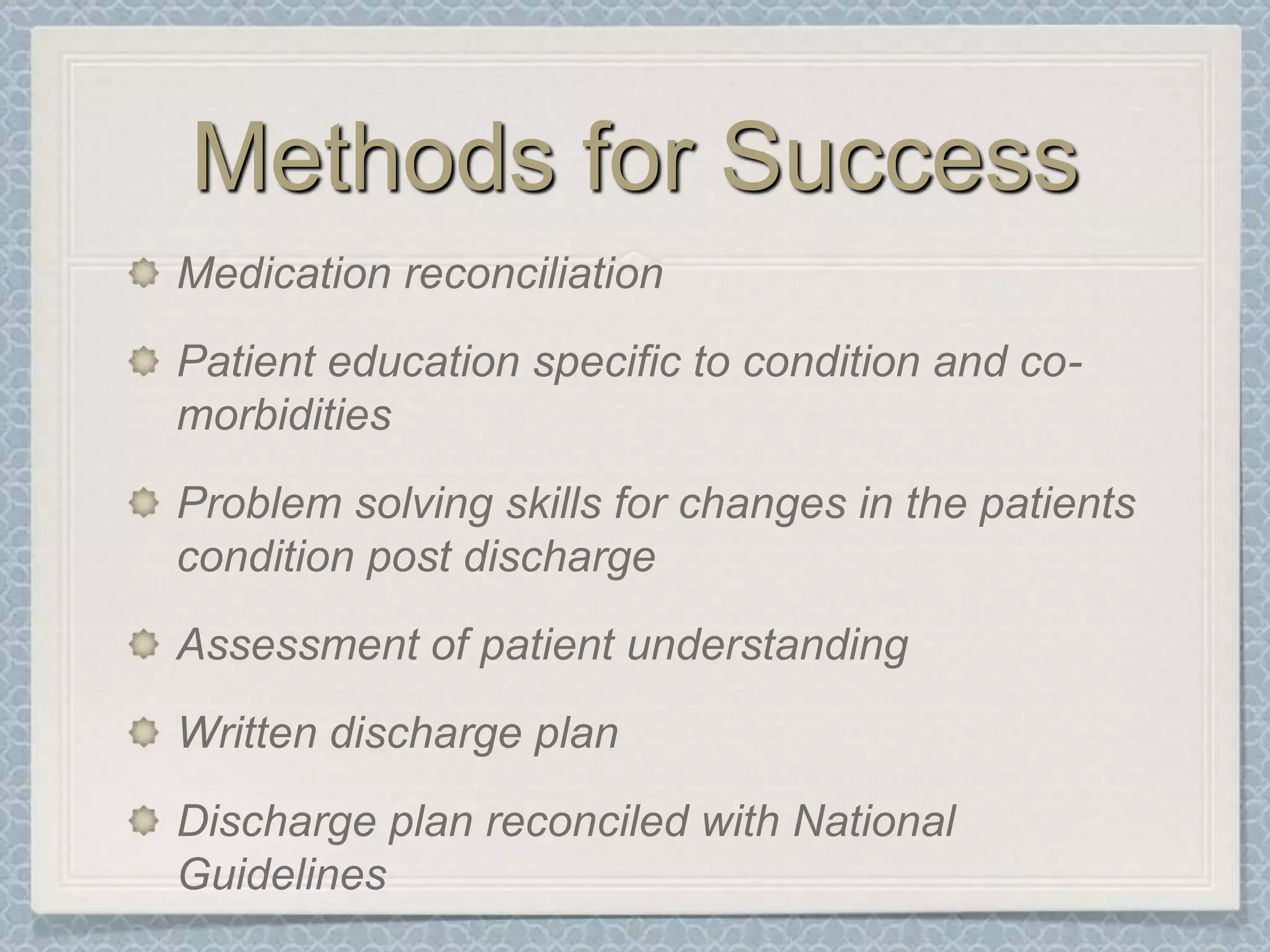
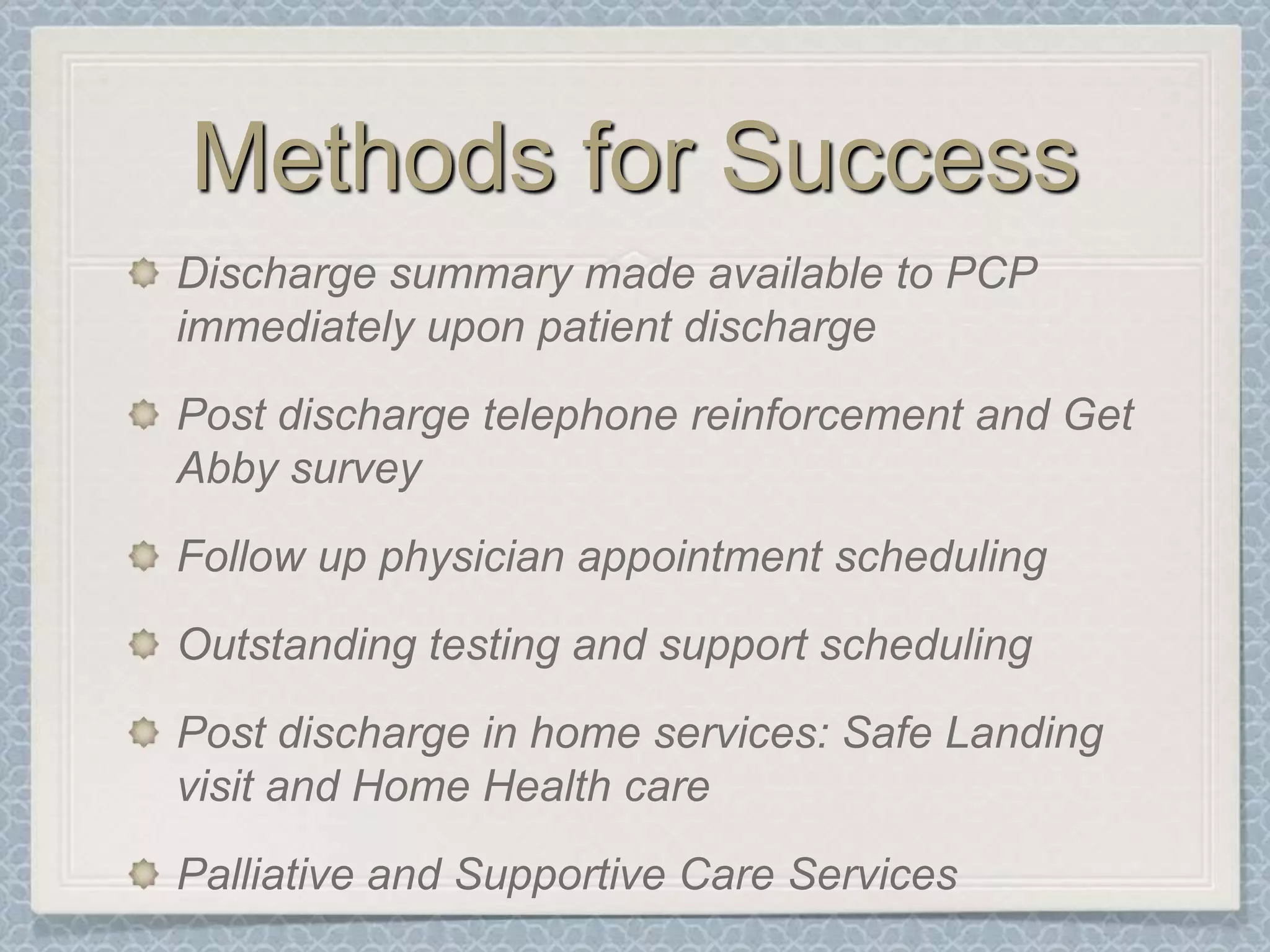
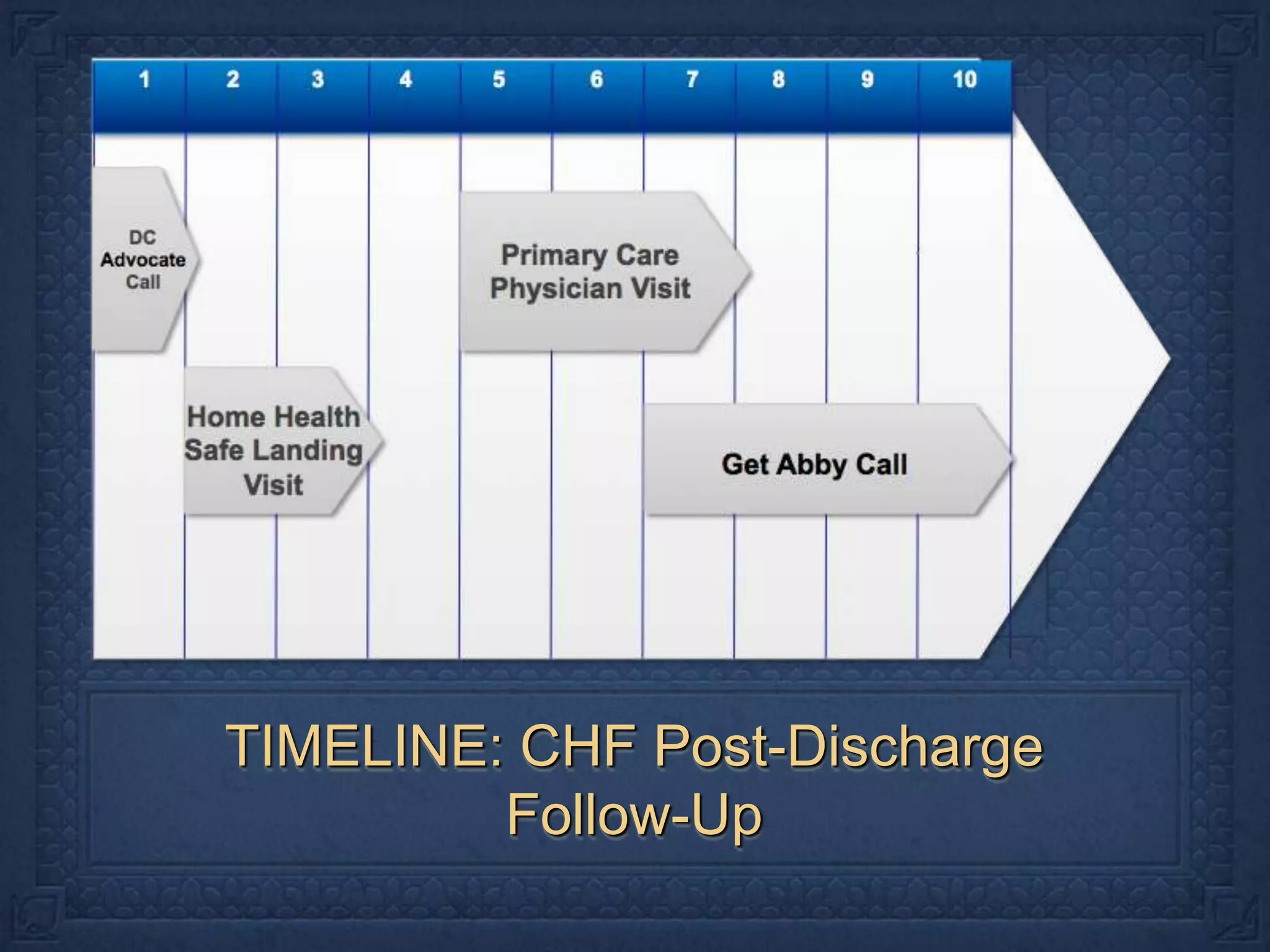
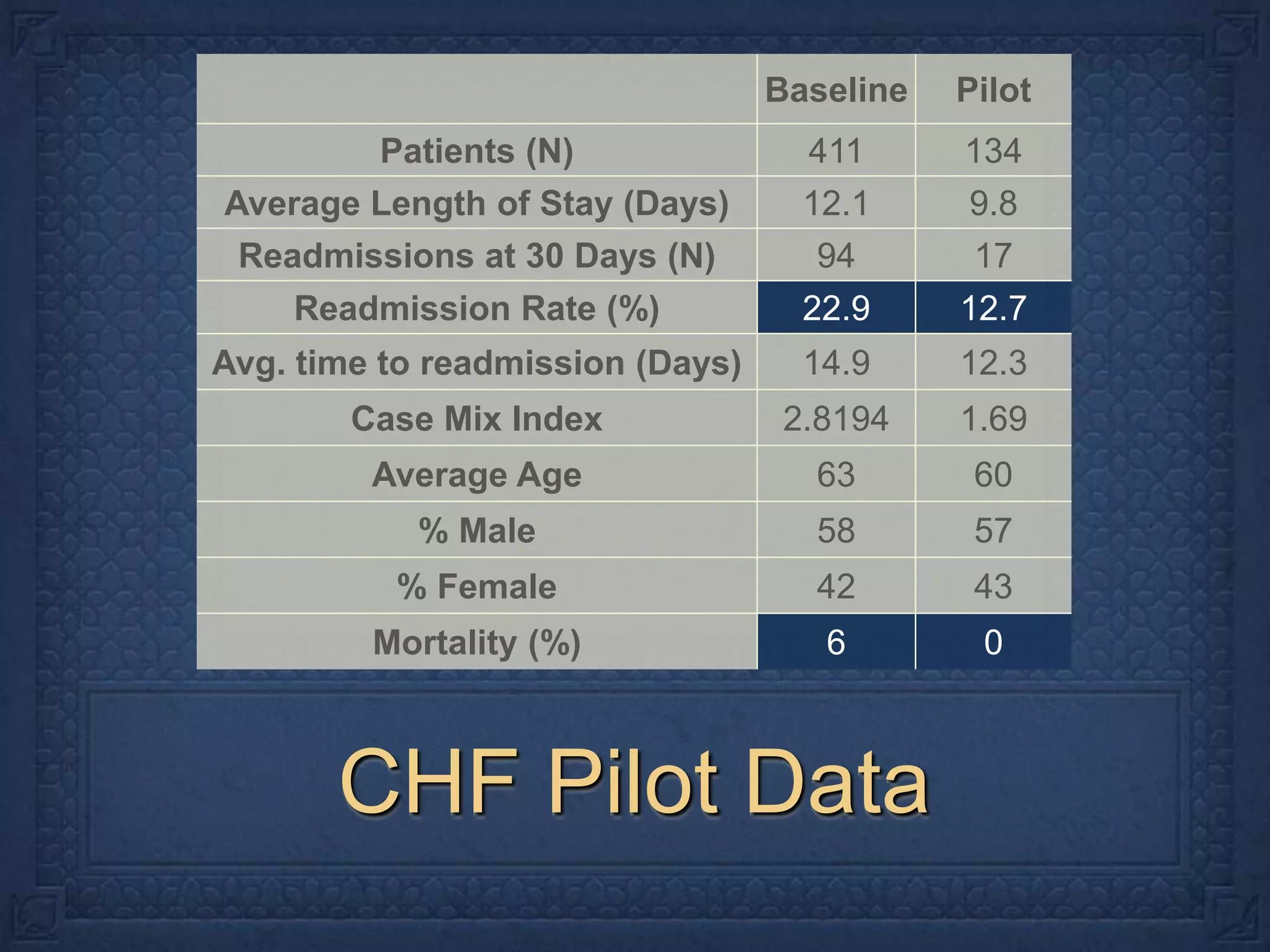
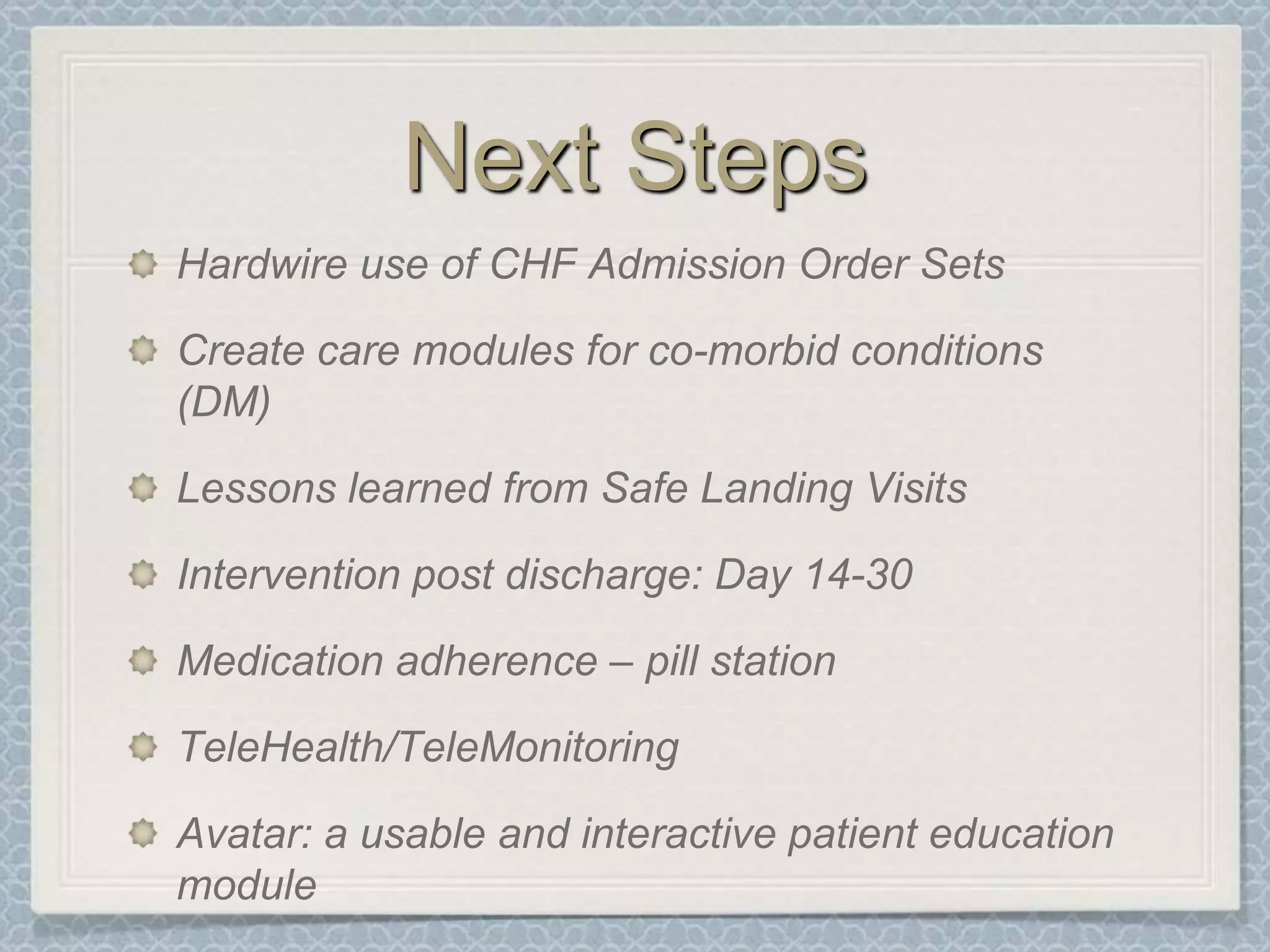
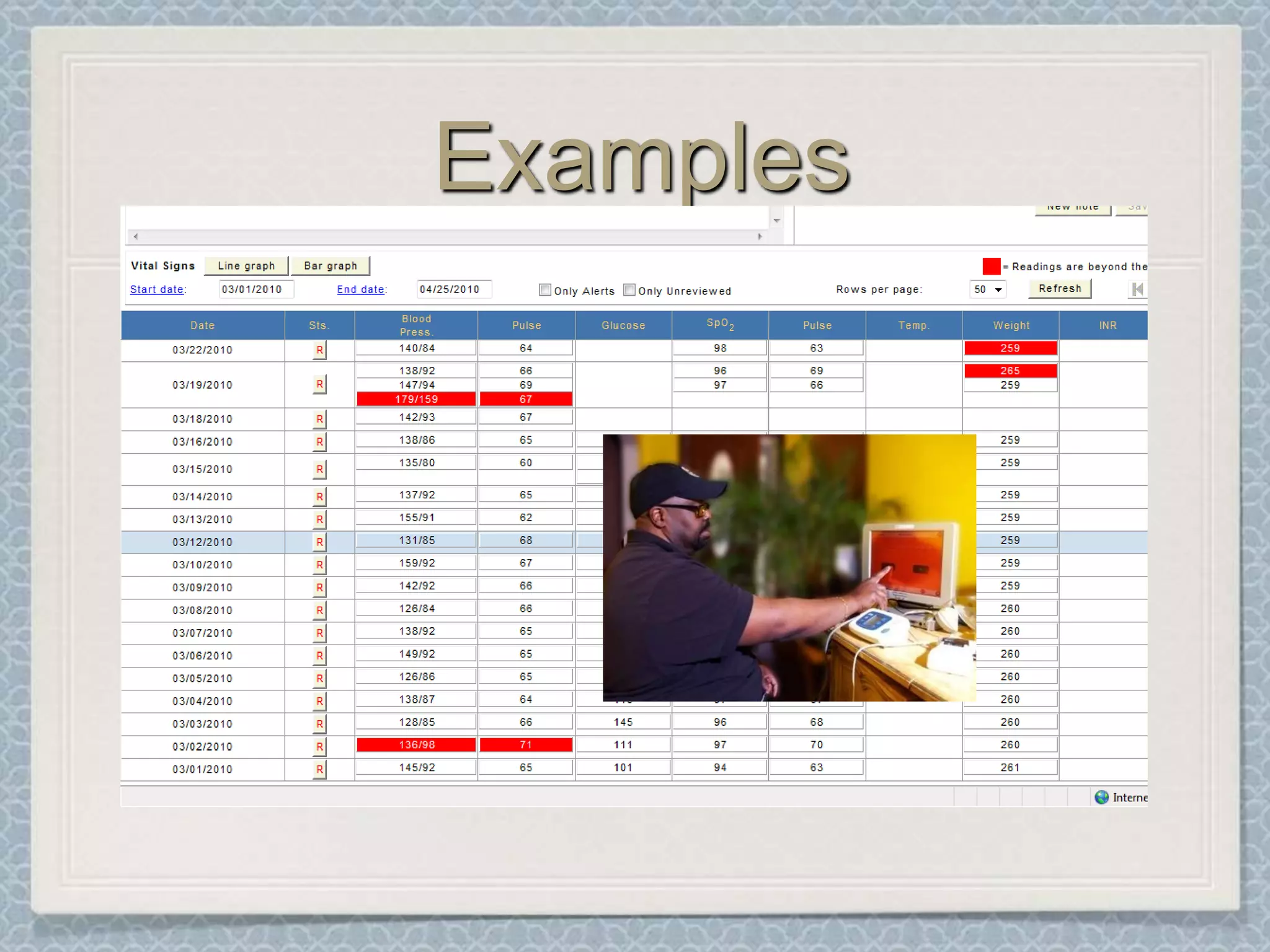
This document discusses using telehealth to manage congestive heart failure (CHF) patients. It provides background on the costs of CHF, highlights some successes of telehealth programs in reducing readmissions and costs. It then describes UPMC's telehealth program for CHF patients, including their goals of reducing readmissions and visits. It outlines their methods, such as medication management and education, and shares some pilot data results. It concludes by discussing next steps like standardizing order sets and exploring telehealth/telemonitoring.