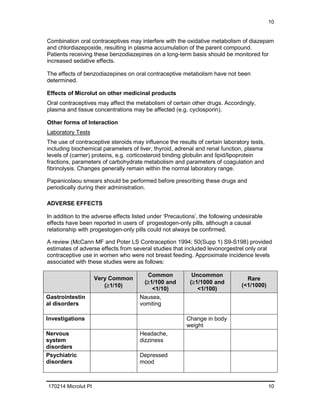
Microlut is an oral contraceptive containing the progestogen levonorgestrel. It prevents pregnancy through changes to the cervical mucus and endometrium that inhibit sperm migration and implantation. While efficacy is slightly lower than combined oral contraceptives, correct usage results in a very low chance of pregnancy. Levonorgestrel is rapidly absorbed and has a half-life of about 20 hours. Microlut is contraindicated in pregnancy, venous thromboembolism, certain cardiovascular conditions, liver tumors, and breast cancer. Precautions include increased risks of circulatory disorders and rare neoplastic effects.