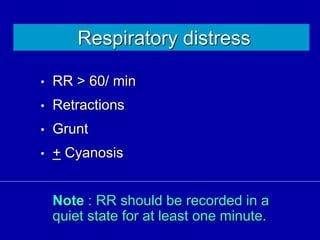
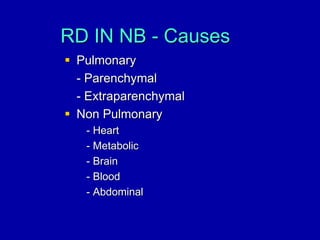
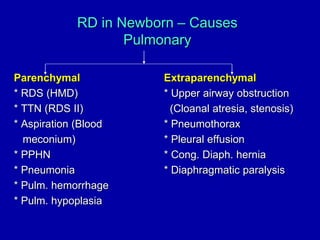
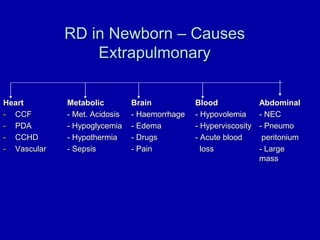
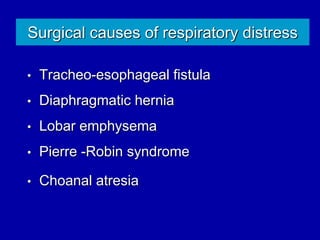
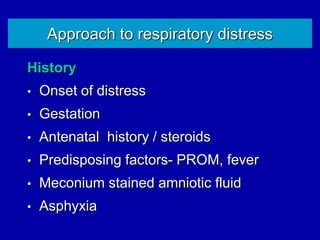
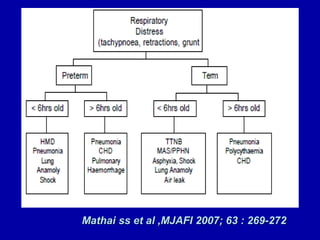
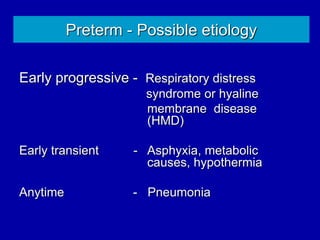
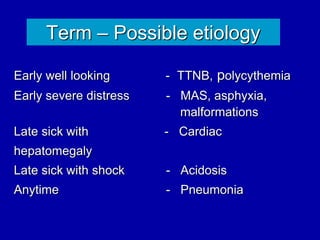
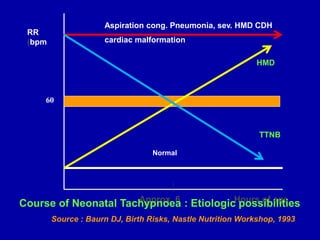
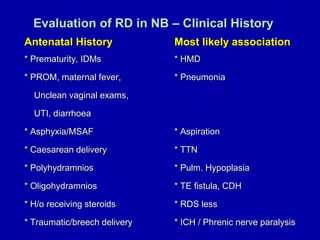
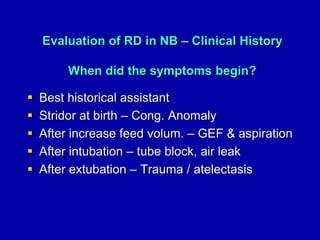
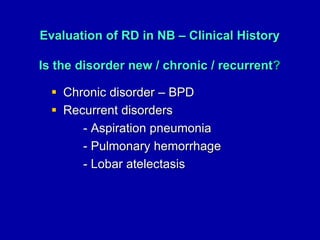
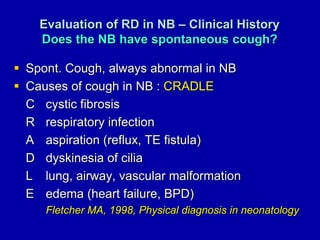
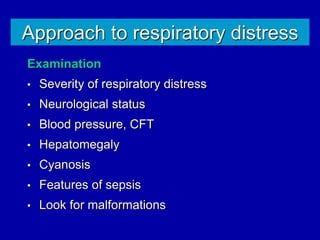
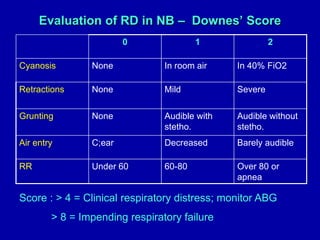
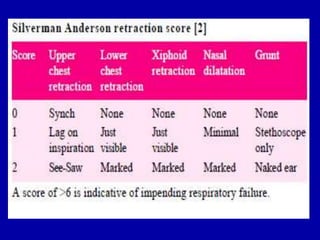
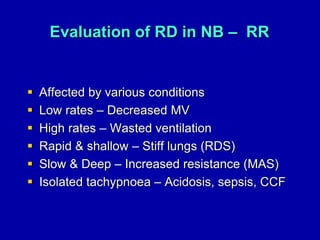
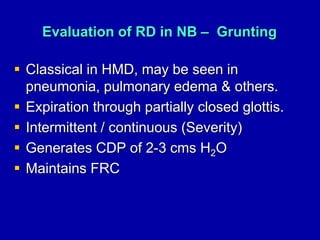
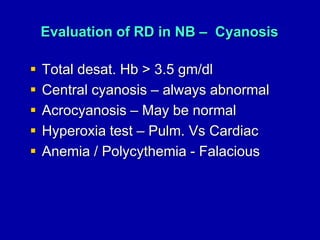
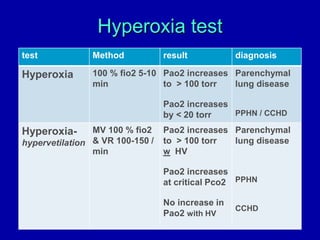
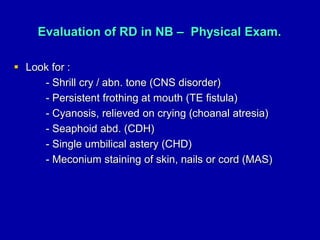
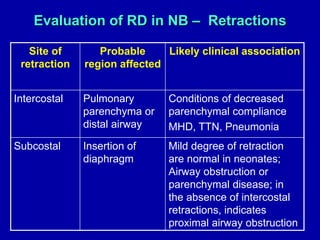
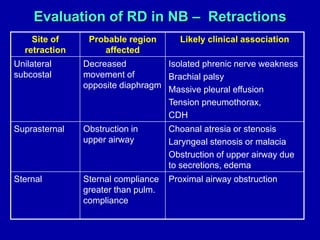
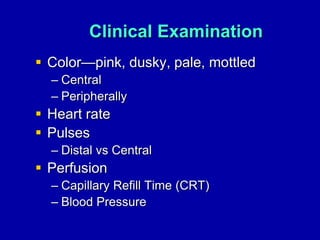
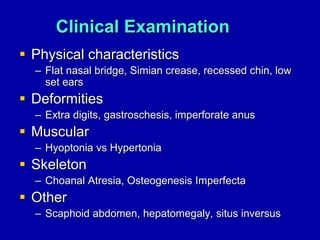
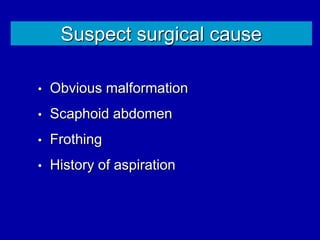
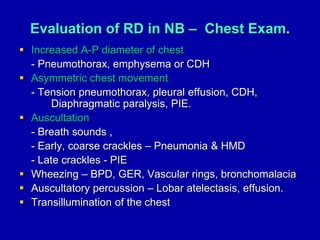
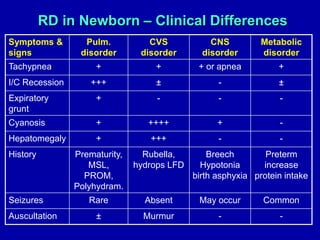
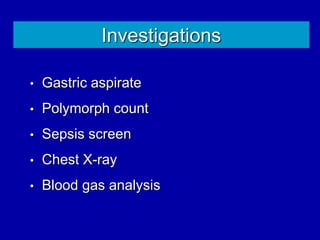
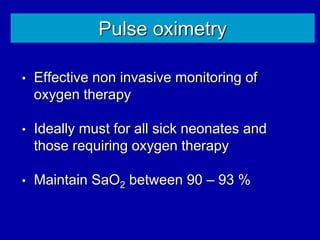
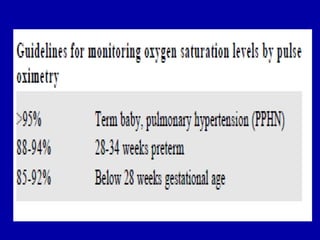
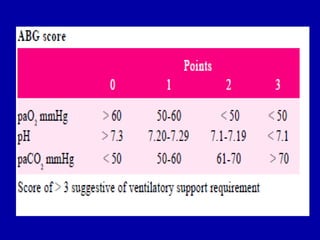
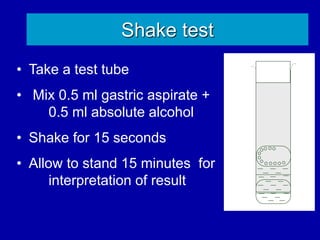
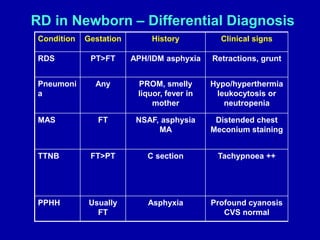
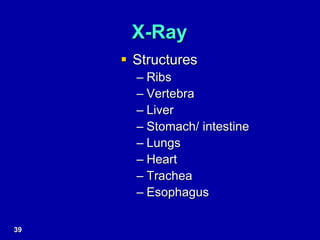
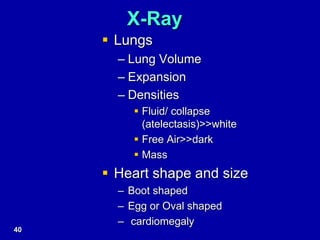
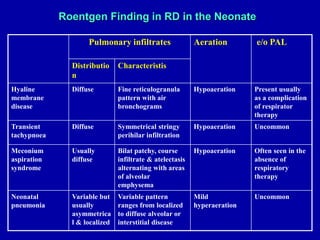
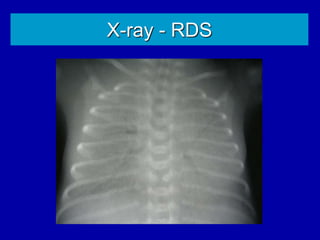
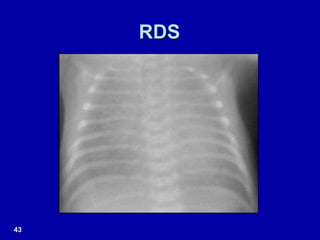
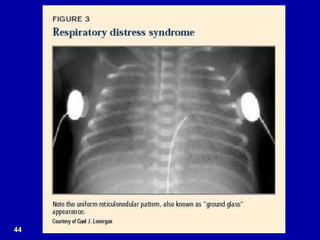
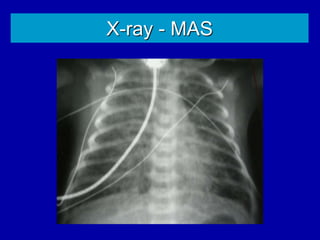
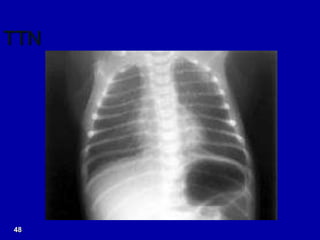
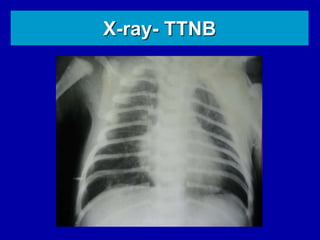
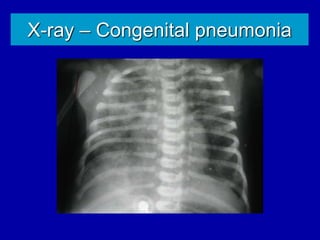
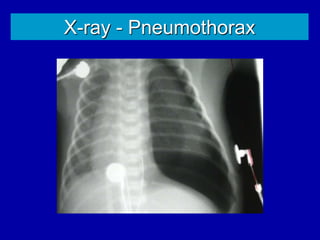
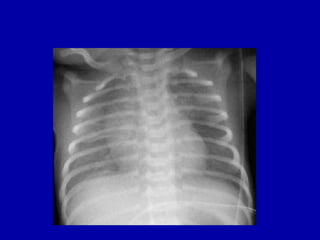
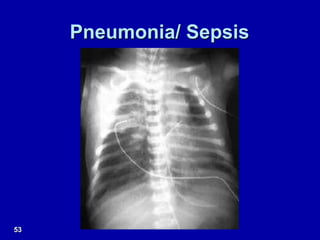
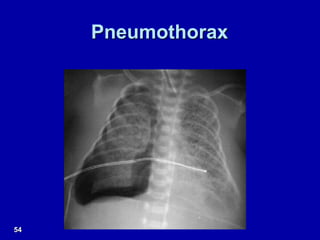
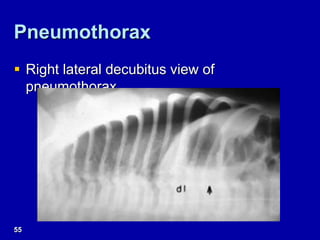
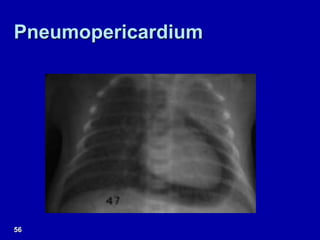
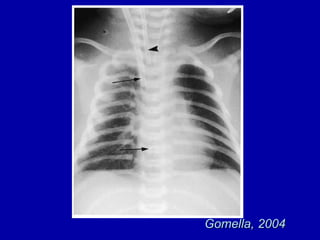
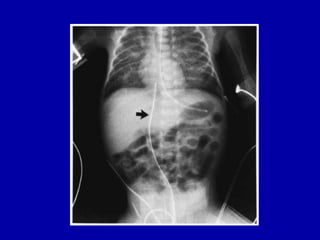
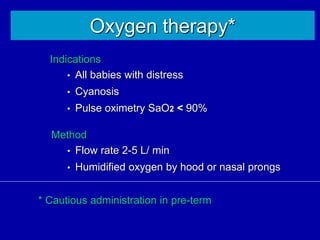
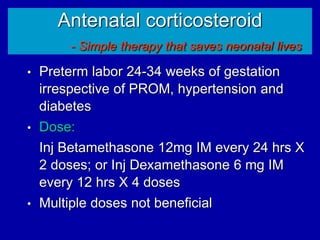
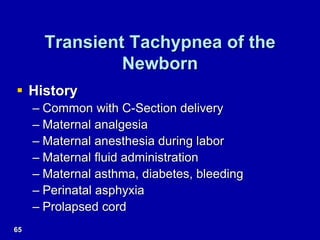
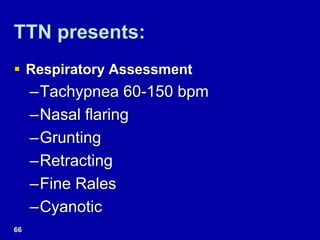
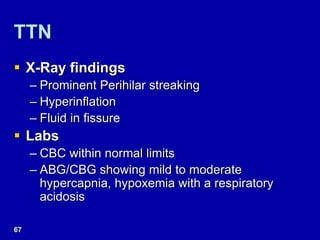
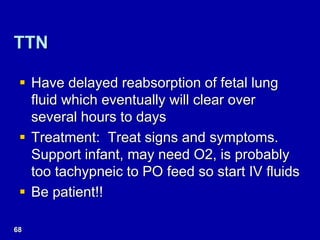
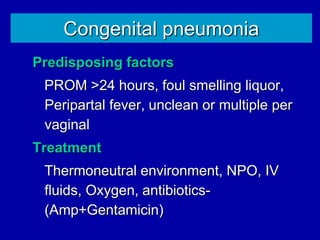
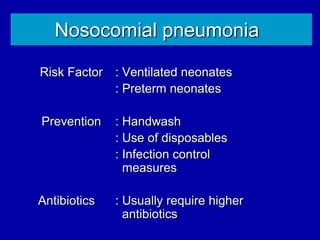
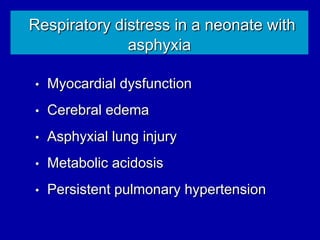
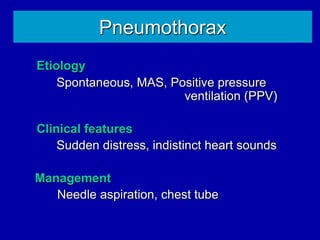
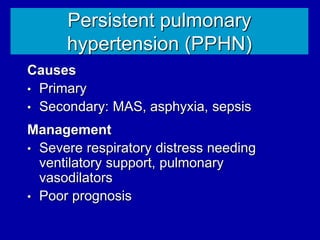
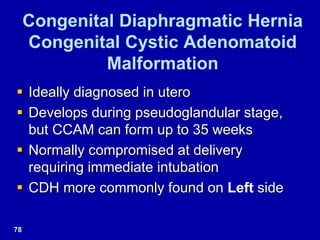
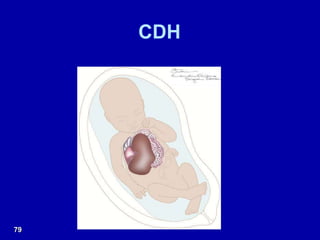
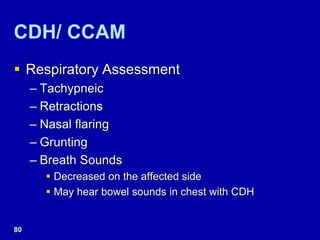
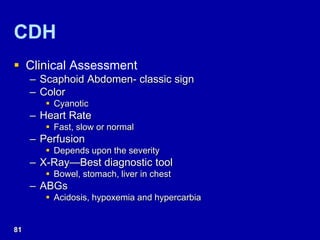
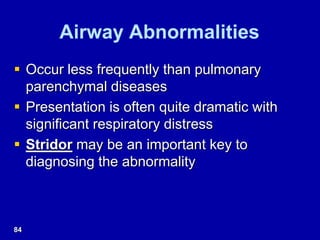
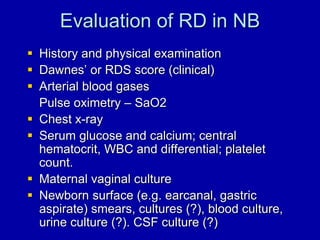
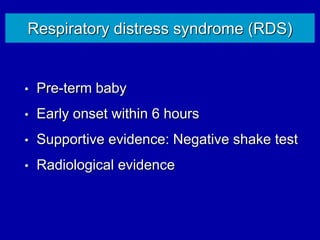
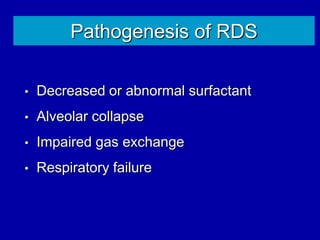
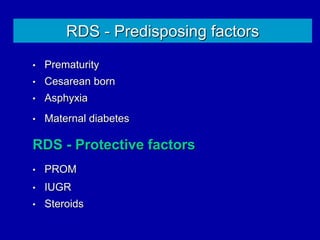
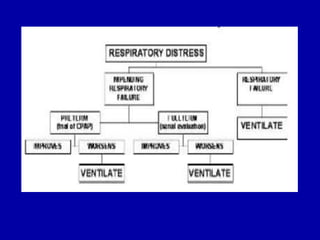
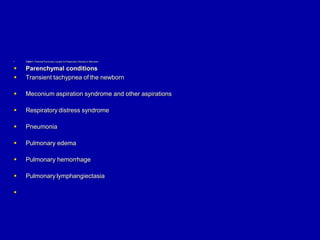
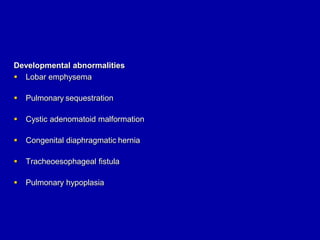
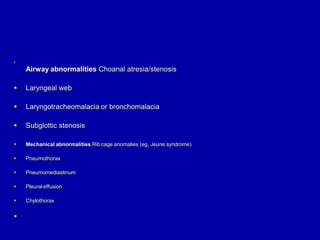
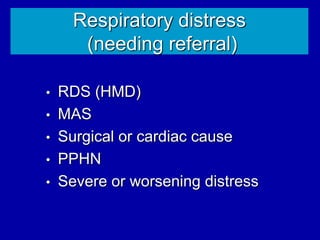
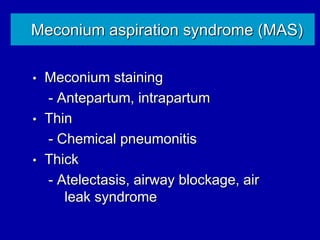
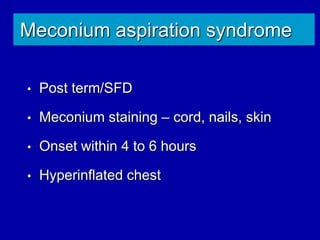
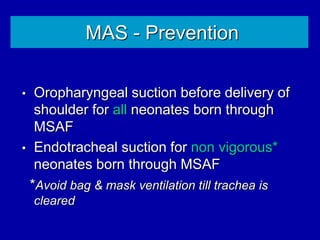
Respiratory distress is a common problem in newborns that can have various causes. It requires early recognition and treatment to prevent morbidity and mortality. The document discusses the causes, clinical presentation, diagnostic evaluation and management of respiratory distress in newborns. Evaluation involves detailed history, physical exam including assessment of respiratory rate, retractions, grunting and cyanosis. Investigations may include chest x-ray, blood gas analysis and sepsis workup. Management is supportive with oxygen therapy, fluid resuscitation and respiratory support as needed. Specific treatments target the underlying condition.