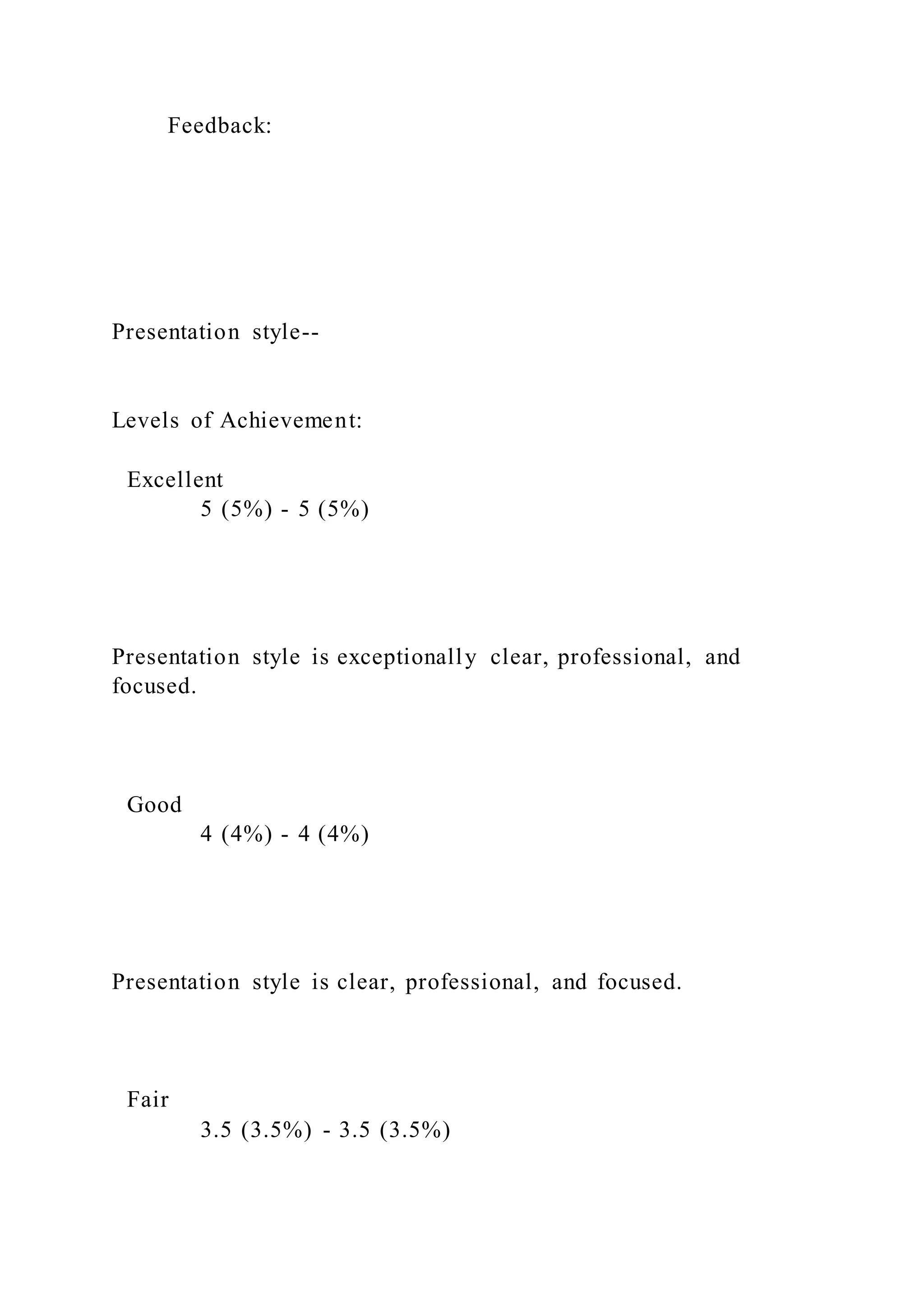
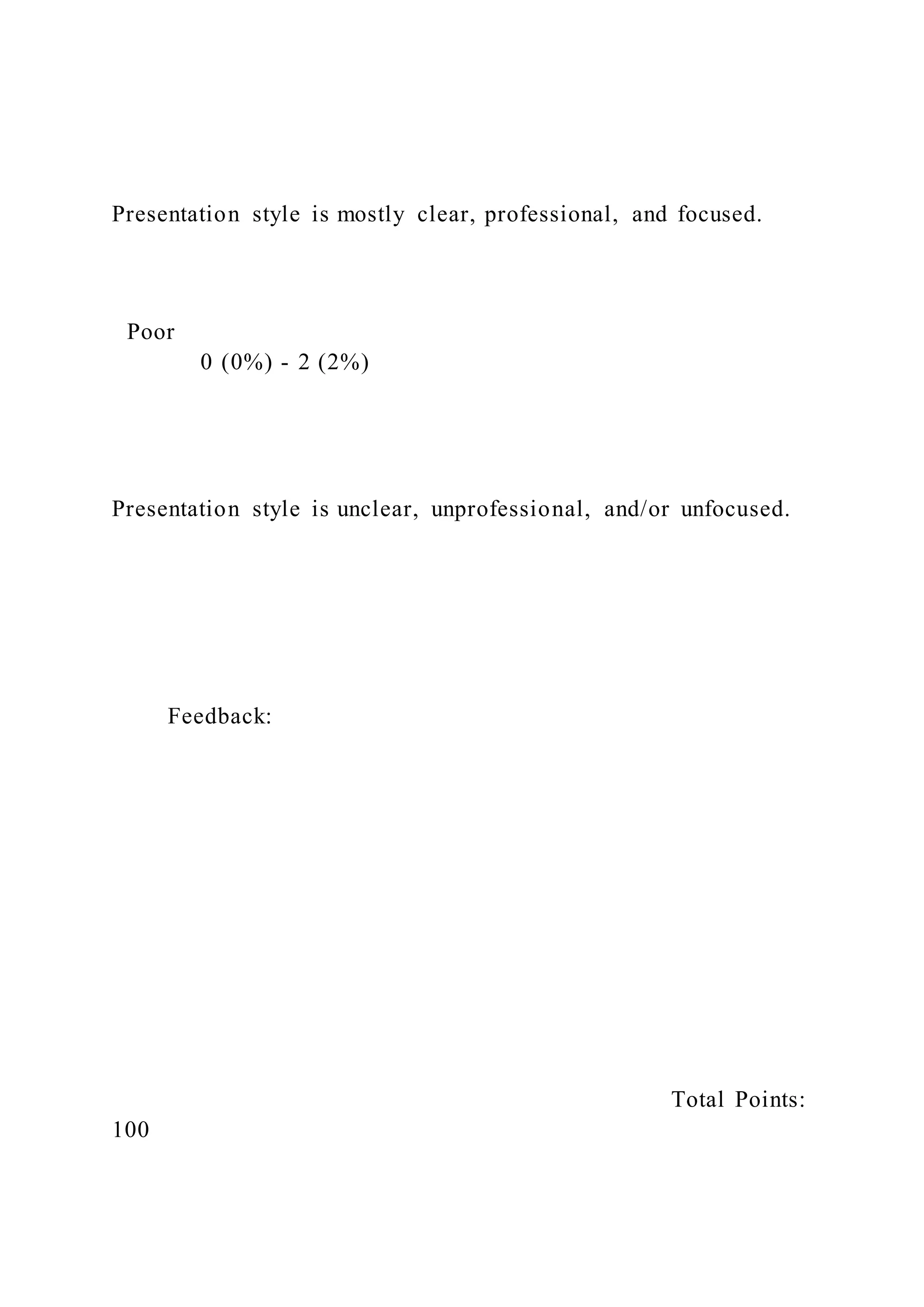
The document outlines the required process recording template for psychiatric evaluations, detailing sections for client introduction, session goals, dialogue analysis, and personal reflections. It emphasizes symptom documentation, differential diagnoses, and planning for treatment based on assessed needs. Additionally, it includes instructions for creating a comprehensive psychiatric evaluation note while adhering to assessment standards and ethical considerations.