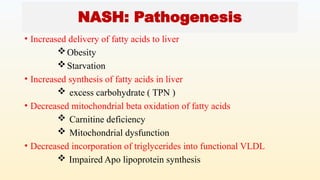
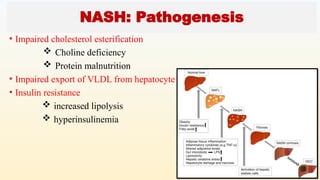
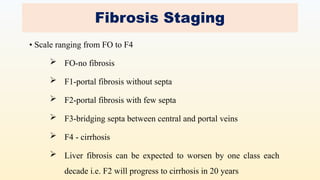
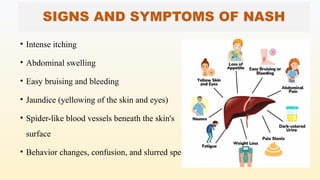
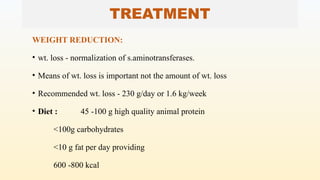
Non-alcoholic steatohepatitis (NASH) is a liver disease characterized by fat accumulation, inflammation, and potential liver damage in individuals who do not abuse alcohol, often linked to obesity, diabetes, and certain metabolic disorders. Diagnosis is confirmed through clinical history, imaging, and liver biopsy, while treatment focuses on lifestyle changes such as weight loss and dietary modifications, as there is no standard medication regimen. NASH increases the risk of cirrhosis, liver failure, and cancer, emphasizing the need for preventive measures through healthy habits.