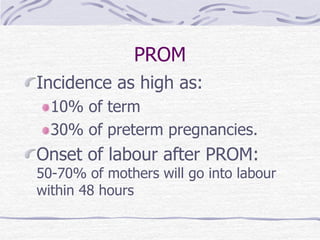
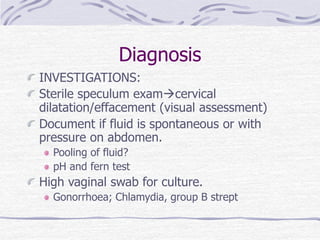
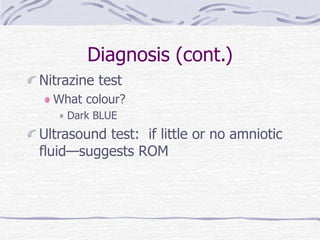
Premature rupture of membranes (PROM) refers to rupture of membranes before the onset of labor. It increases risks of infection and prematurity for the fetus. Risk factors include prior PROM, smoking, and infections. Diagnosis involves confirming fluid leakage and ruling out infection through tests and monitoring. For preterm PROM, antibiotics and steroids may be given and the pregnancy monitored until delivery is imminent. Management focuses on preventing infection by limiting exams and monitoring for signs of infection, with induction typically occurring near term.