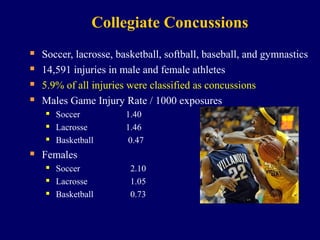
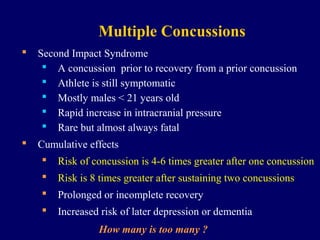
This document discusses concussions in high school and collegiate sports. It reports that over 50% of concussed high school football players do not report their injuries. Among collegiate sports, concussion rates are highest in soccer, lacrosse, and basketball for both males and females. There are misperceptions about concussions among players, coaches, parents, and medical staff regarding return to play timelines. Concussions are classified as brain injuries rather than by severity. Multiple concussions increase long term risks. Strict rest and a gradual return to play protocol under medical supervision are recommended for proper concussion management and recovery.