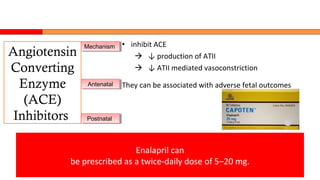
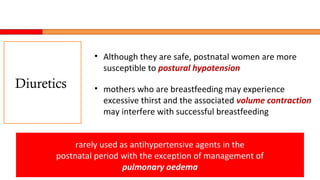
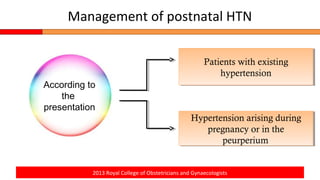
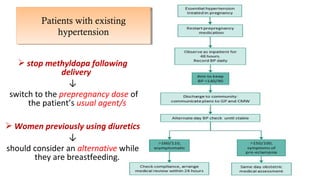
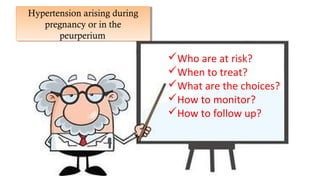
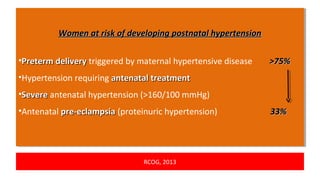
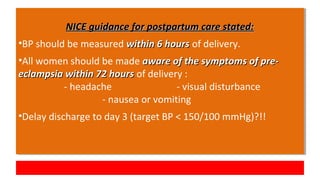
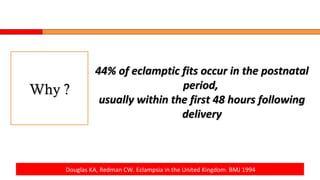
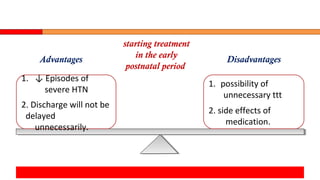
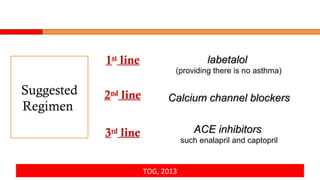
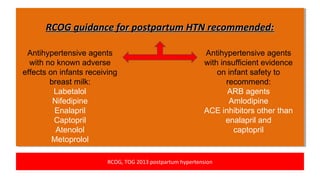
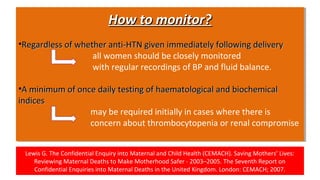
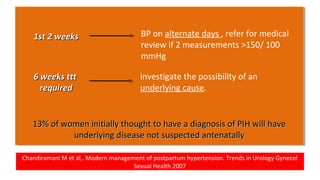
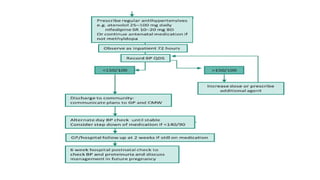
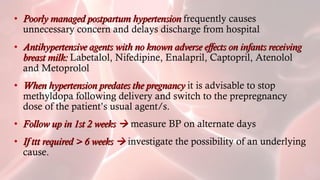
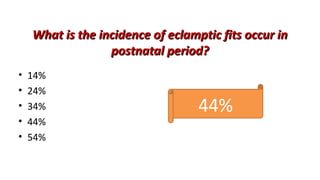
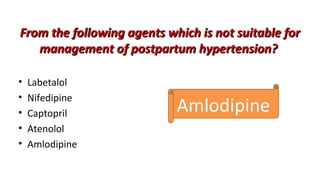
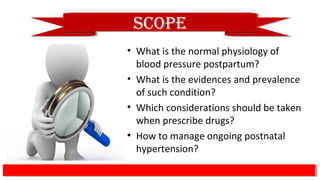
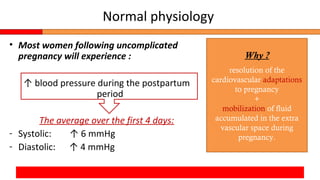
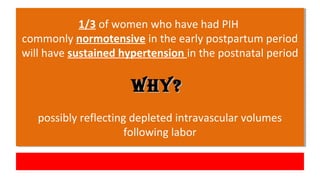
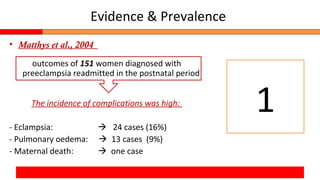
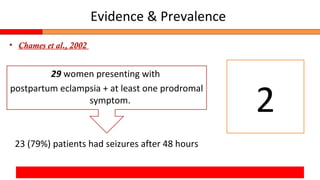
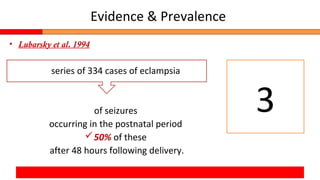
Postpartum hypertension can occur in up to 1/3 of women with gestational hypertension or preeclampsia. Close monitoring of blood pressure and symptoms is important as 44% of eclamptic fits occur within 48 hours of delivery. First-line treatment includes labetalol, calcium channel blockers like nifedipine, and ACE inhibitors like enalapril which are considered safe for breastfeeding. Women at high risk require frequent monitoring of blood pressure and labs initially. Guidelines recommend follow up within 2 weeks and evaluating for underlying conditions if treatment is needed over 6 weeks.

![• inhibiting Ca influx into vascular myoctyes
inhibiting vasoconstriction + ↓ vascular resistance
• Minimal effects on cardiac conduction and heart rate
• minimal excretion into breast milk
Nifedipine (slow release [SR]) is the most
commonly prescribed calcium channel blocker and can
initially be prescribed at a dose of 10–20 mg twice daily
Calcium
Channel
Blockers
MechanismMechanism
BenefitsBenefits
PostnatalPostnatal](https://image.slidesharecdn.com/postpartumhtn-170603210633/85/Postpartum-hypertension-16-320.jpg)