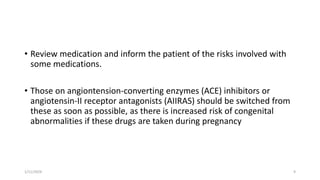
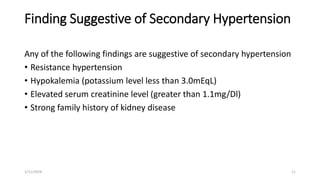
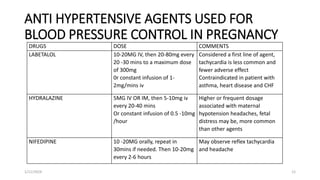
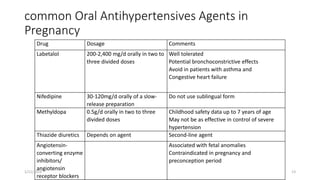
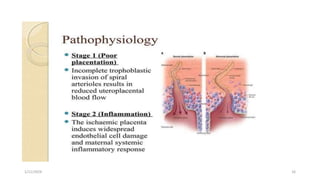
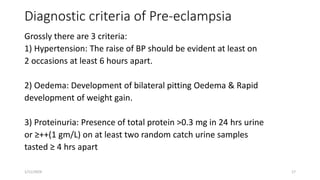
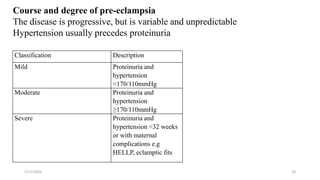
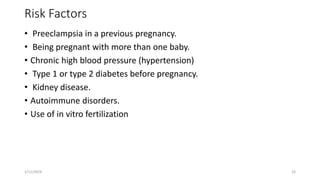
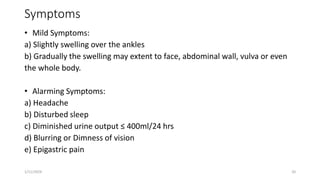
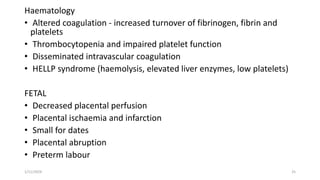
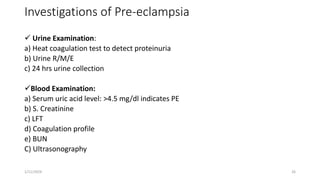
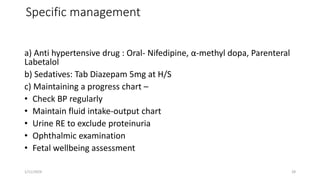
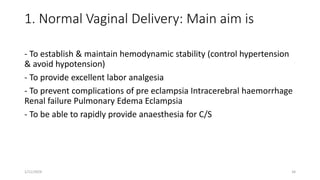
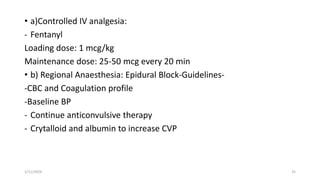
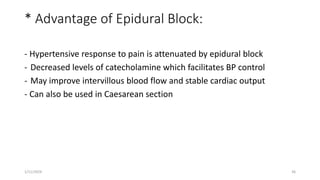
The document discusses chronic hypertension in pregnancy and pre-eclampsia. It defines chronic hypertension as hypertension present before 20 weeks of gestation. Risk factors for chronic hypertension include age over 40, duration of hypertension over 15 years, high blood pressure levels, and medical disorders. Effects on the pregnancy include superimposed pre-eclampsia, IUGR, and stillbirth. Prenatal care includes tests to rule out other conditions and monitor the pregnancy. Pre-eclampsia is characterized by new hypertension and proteinuria after 20 weeks of gestation in a previously normotensive woman. It can lead to maternal and fetal complications if not monitored and managed properly. Management involves hospitalization, medication, and delivery depending on severity and