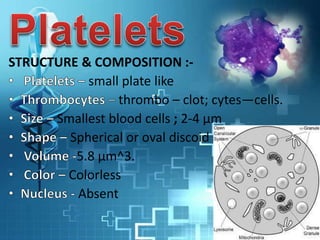
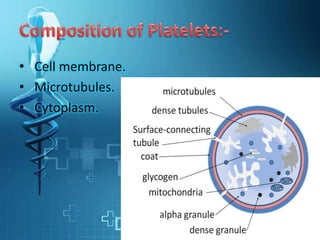
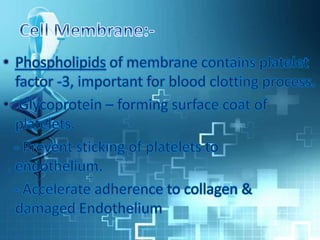
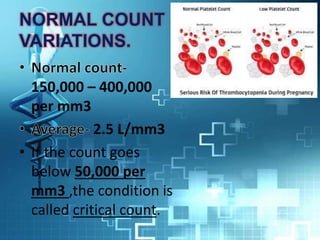
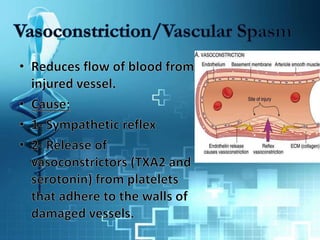
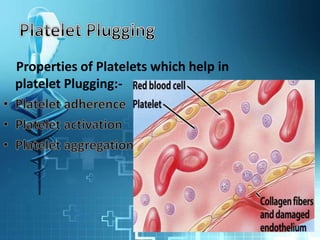
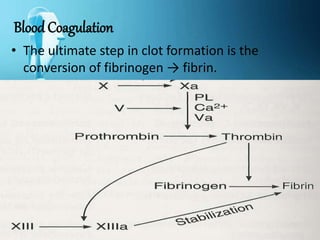
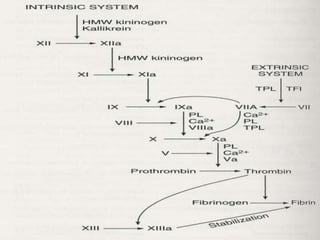
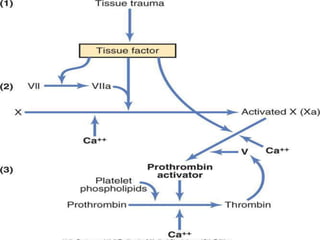
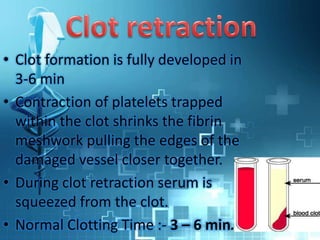
Platelets are the smallest blood cells that help with hemostasis and clot formation. They are discoid in shape and contain various organelles. Platelets have properties like aggregation, agglutination, and adhesiveness which allow them to stick together and to sites of injury to form a platelet plug. This is the first step in hemostasis. The blood coagulation process involves the intrinsic and extrinsic pathways which ultimately result in the conversion of fibrinogen to fibrin to form a clot. Platelets also assist with clot retraction through contraction.