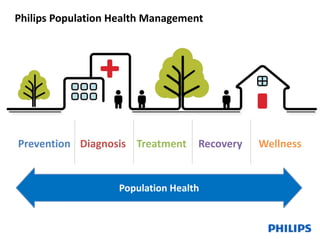
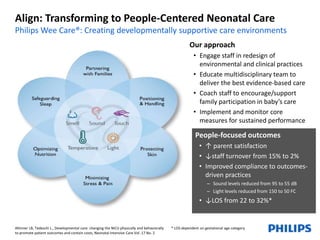
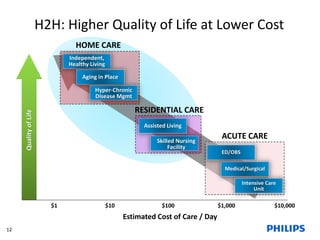
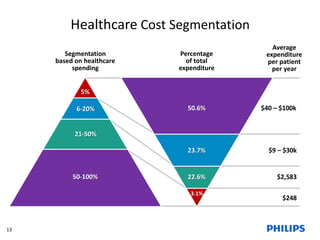
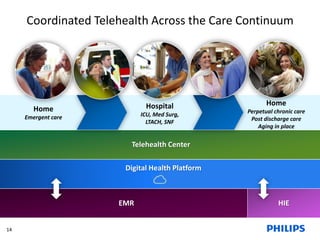
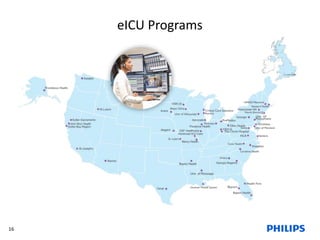
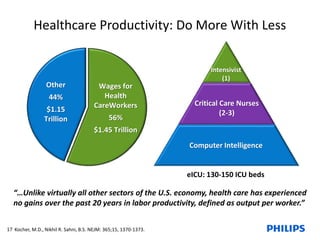
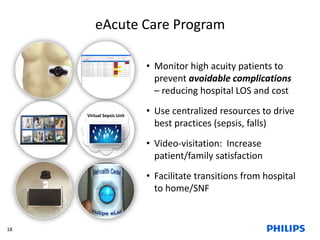
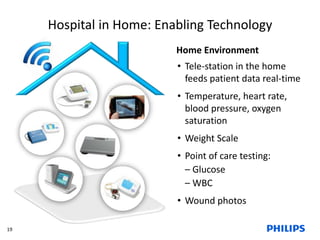
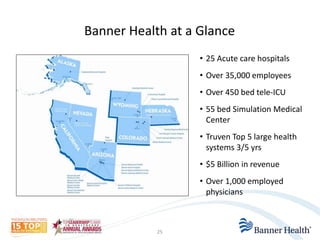
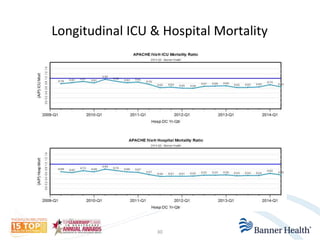
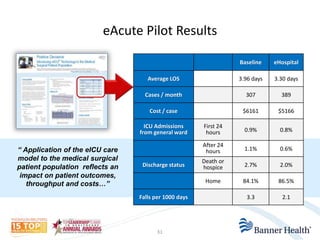
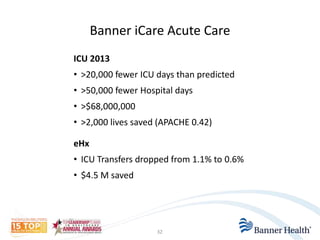
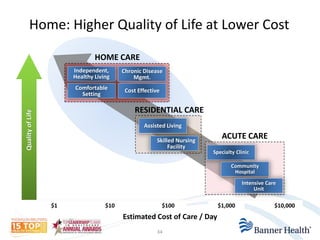
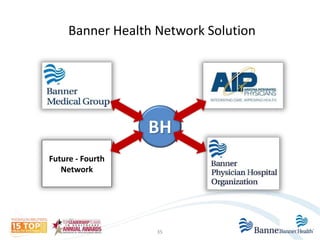
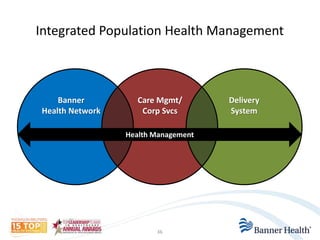
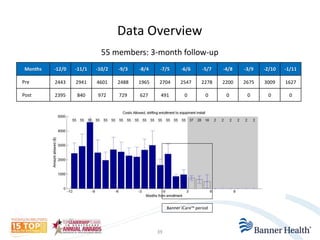
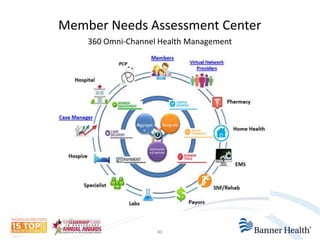
The document discusses strategies for transforming healthcare delivery through population health management, care coordination, and virtual care technologies. It provides examples of how partnerships between healthcare organizations and technology companies have implemented programs utilizing telehealth, remote patient monitoring, and digital platforms to improve outcomes, lower costs, and enable aging in place. Case studies demonstrate how these approaches have reduced hospital admissions and lengths of stay, ICU transfers, mortality rates, and costs while improving quality of life.