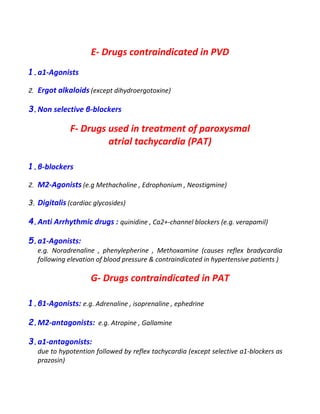
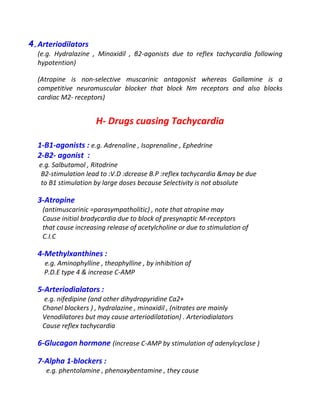
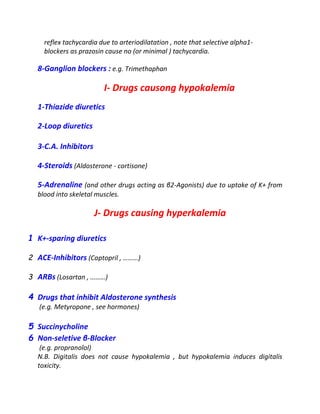
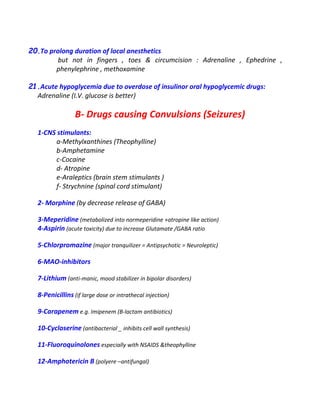
This document lists various drugs categorized by their pharmacological actions and effects. It discusses drugs that act by inhibiting enzymes, including drugs that inhibit phosphodiesterase enzymes. It also categorizes drugs based on their effects on the gastrointestinal system and liver, such as drugs that cause hepatotoxicity, diarrhea, constipation, nausea, and vomiting. Additionally, it outlines drugs and their effects on the cardiovascular system, including those that cause bradycardia, postural hypotension, and their uses in treating postural hypotension and peripheral vascular disease.