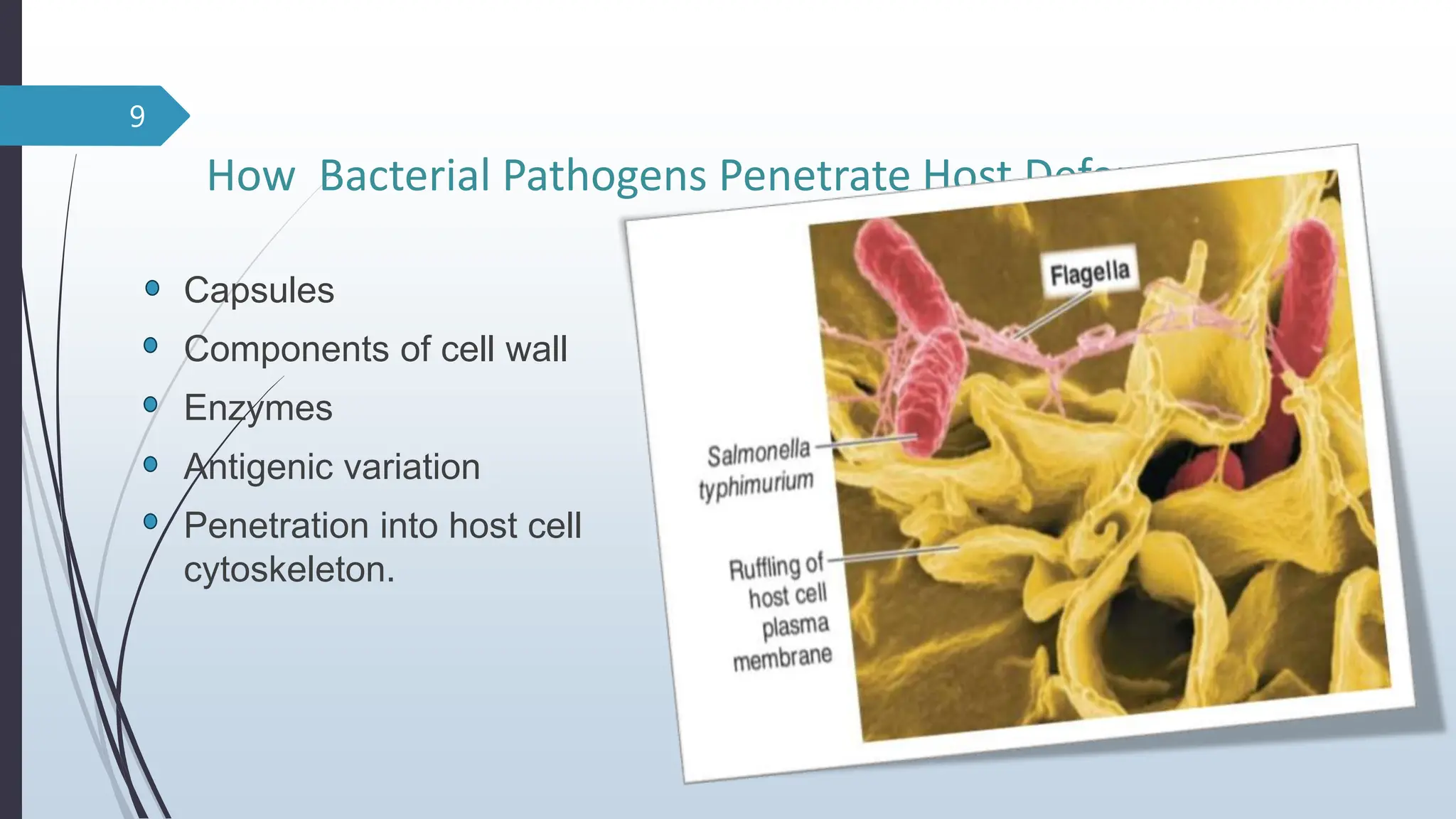
The document discusses microbial pathogenesis, detailing how microorganisms cause infections and damage host cells through various mechanisms such as adherence, evasion of immune responses, and production of toxins. It also outlines the portals of entry for pathogens, factors influencing infection severity, and the different ways various pathogens like bacteria, viruses, fungi, and parasites can affect host health. Additionally, it highlights the role of the immune response in the manifestation of symptoms in certain diseases.