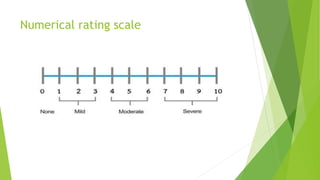
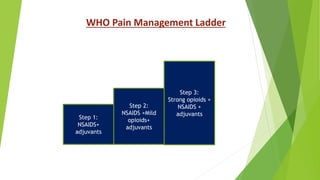
This document provides information about pain, including its definition, nature, components, types, categories, assessment, and management. It defines pain as a subjective experience associated with actual or potential tissue damage. Pain can be acute, lasting less than 6 months, or chronic, lasting more than 6 months. Assessment involves evaluating location, quality, severity, and other factors. Management includes both pharmacological interventions like analgesics and non-pharmacological methods such as heat/ice therapy, distraction, and massage.