This document discusses drugs that act in the central nervous system, focusing on opioid analgesics and antagonists. It describes the mechanisms of action, effects, uses, and interactions of opioids. The key points are:
- Opioids produce analgesia by interacting with opioid receptors in the CNS and peripheral tissues, and have other effects like sedation, respiratory depression, and constipation.
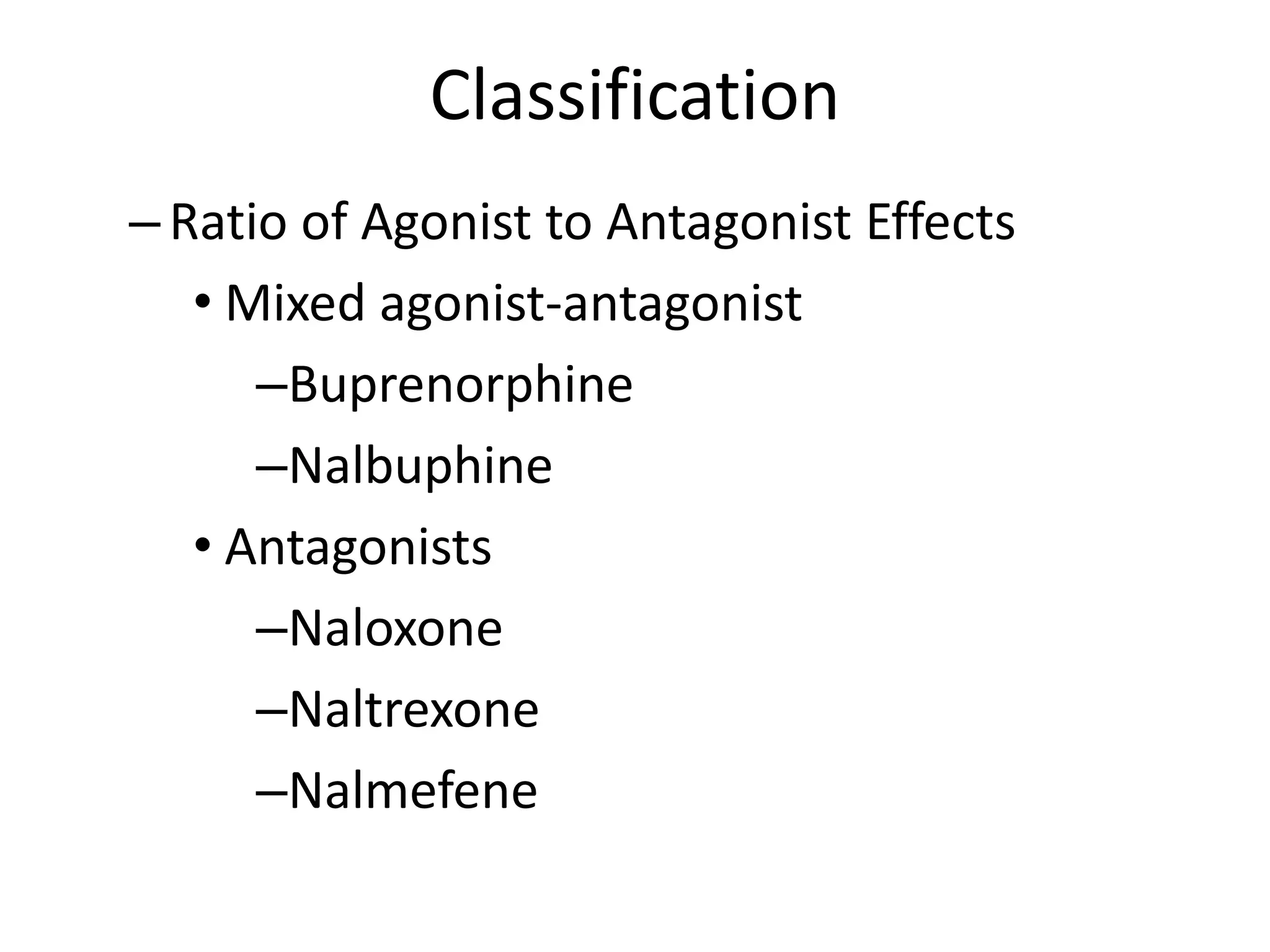
- They are classified based on their affinity for opioid receptors as agonists, mixed agonist-antagonists, or antagonists.
- Common uses include treatment of moderate to severe pain, cough suppression, and diarrhea. Methadone is used to manage opioid dependence.
- Adverse effects include nausea, respiratory