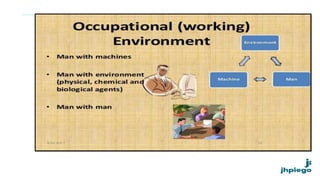
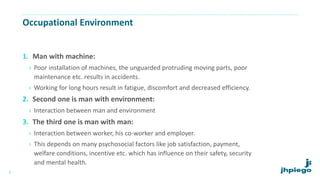
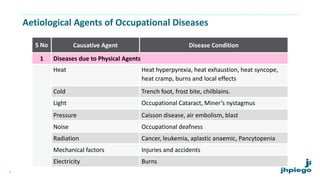
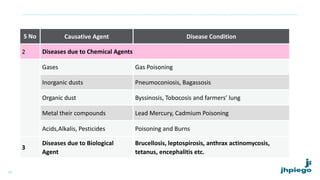
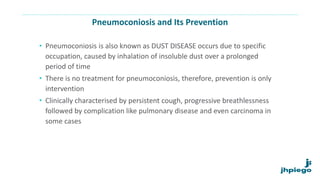
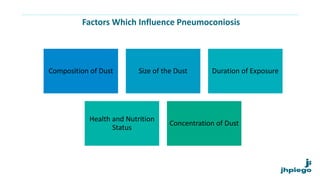
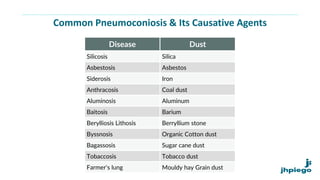
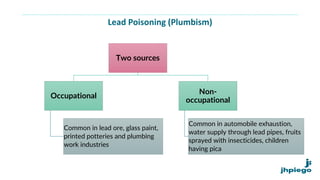
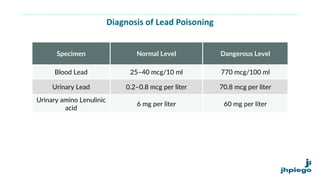
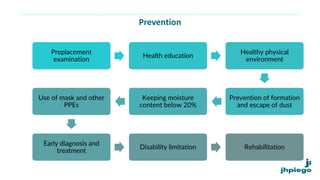
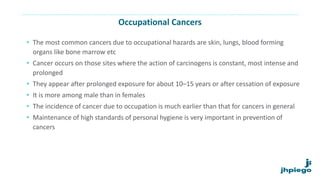
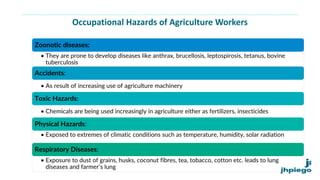
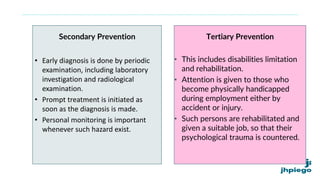
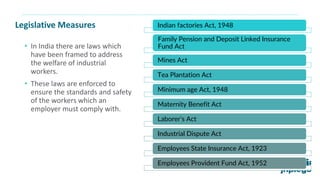
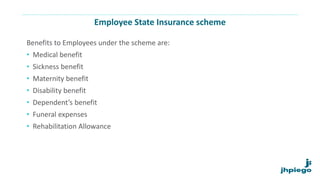
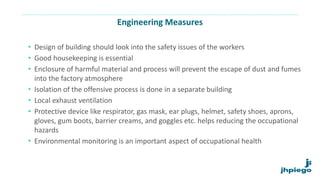
The document discusses occupational diseases and hazards. It notes that there are over 100 million occupational injuries worldwide each year according to WHO, including 17 million non-fatal and 45,000 fatal injuries in India alone. It defines occupational health and lists factors that can affect worker health like physical, chemical, biological, and psychosocial hazards. Common occupational diseases mentioned include pneumoconiosis, lead poisoning, and cancers. The document outlines preventive measures against occupational hazards including pre-placement exams, engineering controls, protective equipment, legislation, and the roles of health providers in prevention, treatment, and rehabilitation.