This document discusses effective communication strategies for interdisciplinary discharge planning. It emphasizes the importance of communication between healthcare team members and patients during the discharge planning process. Key points include:
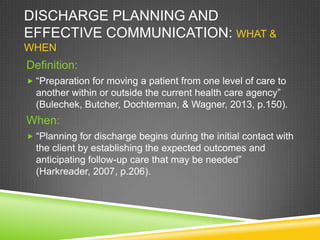
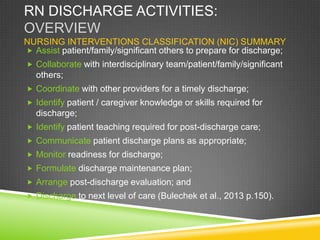
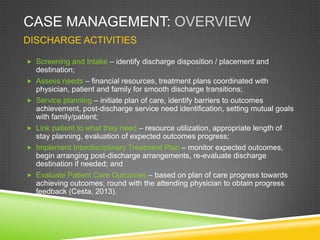
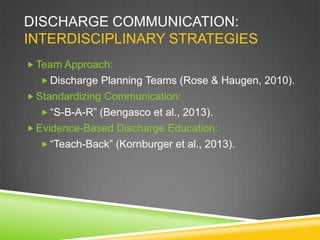
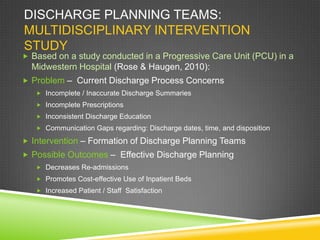
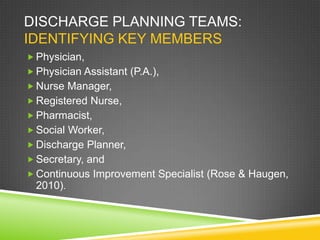
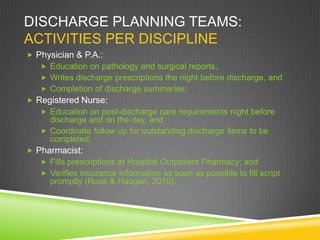
- Discharge planning should begin upon admission using a team approach involving nurses, physicians, social workers, and other disciplines.
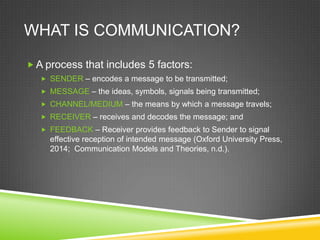
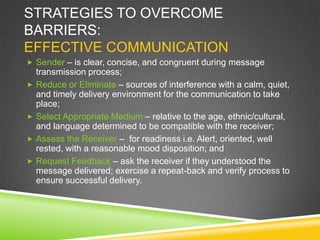
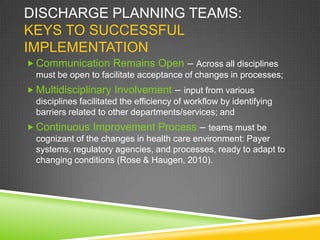
- Standardizing communication tools like SBAR (Situation, Background, Assessment, Recommendation) can help ensure all relevant information is conveyed accurately between teams.
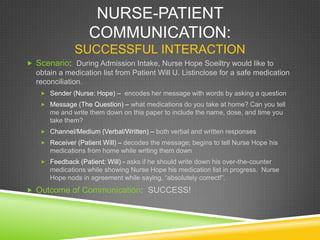
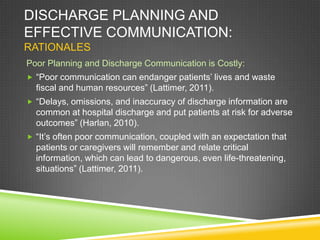
- Using techniques like "teach-back" allows nurses to assess patient and family understanding of discharge instructions before they leave to help prevent errors and readmissions.