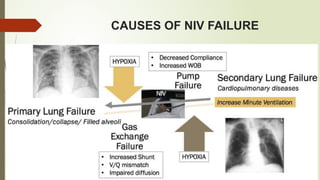
Non-Invasive Ventilation (NIV) is a respiratory support technique that delivers air or oxygen through a mask without the need for intubation. It is commonly used for conditions like chronic obstructive pulmonary disease (COPD), respiratory failure, and sleep apnea. NIV helps reduce work of breathing, improves gas exchange, and prevents complications associated with invasive ventilation, such as infections. There are two main types: continuous positive airway pressure (CPAP) and bilevel positive airway pressure (BiPAP). NIV is preferred in many cases due to its comfort, ease of use, and ability to be administered in hospital and home settings for long-term management.