The document outlines new sepsis guidelines emphasizing the importance of early diagnosis and immediate treatment for sepsis and septic shock, highlighting key diagnostic criteria and risk factors. It includes recommendations for fluid resuscitation, antimicrobial therapy, and supportive care strategies such as the use of vasopressors and ventilation techniques. It also stresses the importance of patient-centered care, including discussions about goals of care and support for families of affected patients.

![ Normal WBC count with greater than 10 percent immature forms
Plasma C-reactive protein more than two standard deviations above the
normal value
Plasma procalcitonin more than two standard deviations above the normal
value
Hemodynamic variables
Arterial hypotension (systolic blood pressure SBP <90 mmHg, MAP <70 mmHg,
or an SBP decrease >40 mmHg in adults or less than two standard deviations
below normal for age)
Organ dysfunction variables
Arterial hypoxemia (arterial oxygen tension [PaO 2 ]/fraction of inspired
oxygen [FiO 2 ] <300)](https://image.slidesharecdn.com/newsepsisguidelines-240520174726-0be14fd2/85/New-sepsis-guidelines-pptx-mmmmmmmmmmm-4-320.jpg)
![ Acute oliguria (urine output <0.5 mL/kg/hr for at least two hours despite
adequate fluid resuscitation)
Creatinine increase >0.5 mg/dL or 44.2 micromol/L
Coagulation abnormalities (international normalized ratio [INR] >1.5 or activated
partial thromboplastin time [aPTT] >60 seconds)
Ileus (absent bowel sounds)
Thrombocytopenia (platelet count <100,000 microL –1 )
Hyperbilirubinemia (plasma total bilirubin >4 mg/dL or 70 micromol/L)
Tissue perfusion variables
Hyperlactatemia (>1 mmol/L)
Decreased capillary refill or mottling](https://image.slidesharecdn.com/newsepsisguidelines-240520174726-0be14fd2/85/New-sepsis-guidelines-pptx-mmmmmmmmmmm-5-320.jpg)

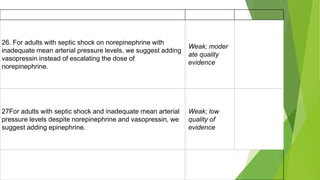
![Surviving sepsis guidelines
1. For hospitals and health systems, we recommend using a performance improvement program for
sepsis, including sepsis screening for acutely ill, high-risk patients and standard operating
procedures for treatment.
2. We recommend against using qSOFA {BP<100,GCS <13,R/R22}.compared with SIRS, NEWS, or
MEWS as a single-screening tool for sepsis or septic shock.{NEW,Strong recommendation}
Modified early warning system news{Mews]
National early warning system news{news}
Quick Sepsis related Organ Failure Assessment](https://image.slidesharecdn.com/newsepsisguidelines-240520174726-0be14fd2/85/New-sepsis-guidelines-pptx-mmmmmmmmmmm-8-320.jpg)












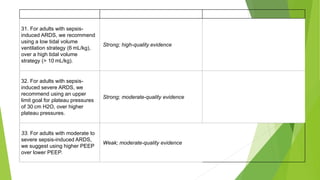
![ 34. When using recruitment maneuvers, we recommend against using
incremental PEEP titration/strategy.
[Strong; moderate-quality evidence]
35. For adults with sepsis-induced moderate-severe ARDS, we recommend
using prone ventilation for greater than 12 hr daily.
[Strong; moderate-quality evidence]](https://image.slidesharecdn.com/newsepsisguidelines-240520174726-0be14fd2/85/New-sepsis-guidelines-pptx-mmmmmmmmmmm-32-320.jpg)