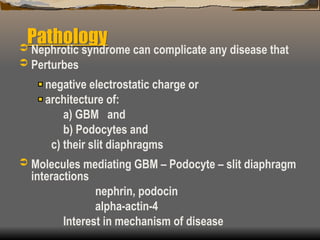
Nephrotic syndrome is characterized by significant proteinuria, hypoalbuminemia, and various metabolic complications, often resulting from glomerular diseases that may be primary or secondary. The document discusses the causes, diagnostic investigations, common histological entities, clinical manifestations, and treatment strategies aimed at managing complications such as infections, hyperlipidemia, and hypercoagulability. Treatment goals include inducing remission, managing symptoms, and preventing long-term complications.
![Glomerular Diseases
1. Various diseases affect the glomerulus
they could be inflammatory or non-
inflammatory
2. Diseases lead to alterations glomerular
permiability [Proteinuria] ; structure
[Histology] ; and function [GRF].](https://image.slidesharecdn.com/nephroticsyndrome-241008091001-93cae592/85/Nephrotic-Syndrome-powerpoint-presentation-2-320.jpg)
![[Contd.] Glomerular Disease
Glomerular disease can be primary [restricted in
clinical manifestation to the kidney, with unknown
cause]
Or secondary (secondary to known primary
conditions or part of a multisystem disease)
E.g. systemic lupus
Vasculitis
HIV / HBV / HCV
Diabetes mellitus](https://image.slidesharecdn.com/nephroticsyndrome-241008091001-93cae592/85/Nephrotic-Syndrome-powerpoint-presentation-3-320.jpg)

![Causes of Nephrotic Syndrome
Idiopathic
Post infectious
Viruses [Hepatitis B, C, HIV, measles, EBV]
Bacteria [streptococcal, syphilis]
Parasites [plasmodiam malarie, schistosoma]
Vasculitis /Collagen [SLE, Wegener’s, Henoch-
Schönlein purpura PAN, Good pasture’s]](https://image.slidesharecdn.com/nephroticsyndrome-241008091001-93cae592/85/Nephrotic-Syndrome-powerpoint-presentation-8-320.jpg)
![Causes of Nephrotic Syndrome
[Contd.]
Systemic diseases [Diabetes Mellitus,
amyloidosis]
Drugs/chemicals [Penicillamine, captopril,
gold, Mg]
Allergy [Drugs, vaccines, stings]
Malignancies – [colon, prostate, lung, breast]](https://image.slidesharecdn.com/nephroticsyndrome-241008091001-93cae592/85/Nephrotic-Syndrome-powerpoint-presentation-9-320.jpg)
![Investigations [Contd.]
4. Cause a) clinical examination
b) ASOT, Anti-DNAse, VDRL,
HBs Ag, HCVAb, HIV Elisa, B/S-
MPs, stool, urine micro Blood
sugar, C3 – levels, ANA ,anti -
GBM, ANCA, Anti PLA 2R Ab
Culture (throat, discharges,
skin, blood urine)](https://image.slidesharecdn.com/nephroticsyndrome-241008091001-93cae592/85/Nephrotic-Syndrome-powerpoint-presentation-11-320.jpg)
![Histologic entities [Common]
Minimal change disease (MCD)
Mesangial proliferative GN
Focal and segmental glomerulosclerosis (FSGS)
Membranous glomerulopathy
Membranoproliferative glomerulonephritis (MPGN)
Diabetic nephropathy
Amyloidosis](https://image.slidesharecdn.com/nephroticsyndrome-241008091001-93cae592/85/Nephrotic-Syndrome-powerpoint-presentation-12-320.jpg)






















