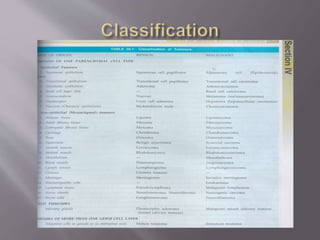
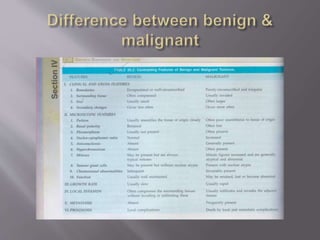
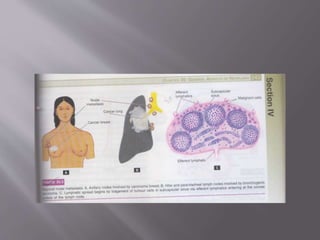
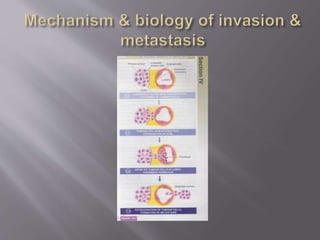
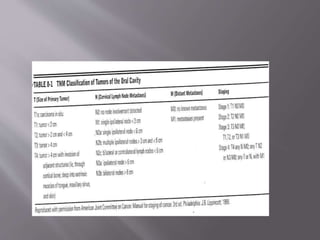
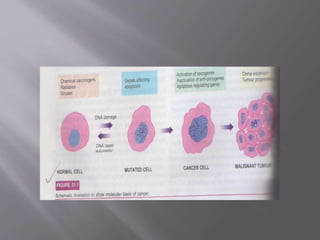
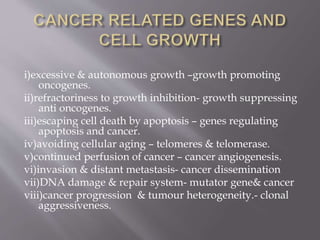
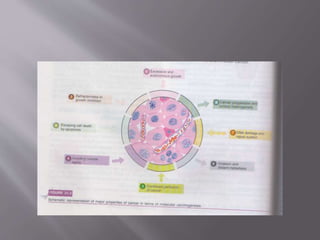
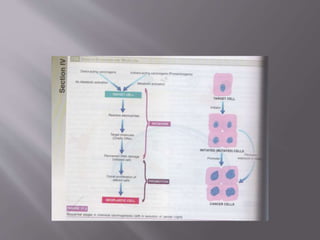
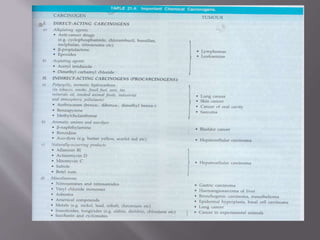
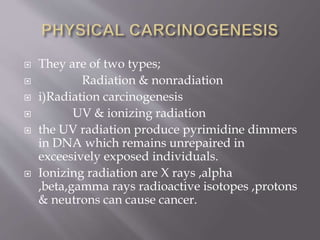
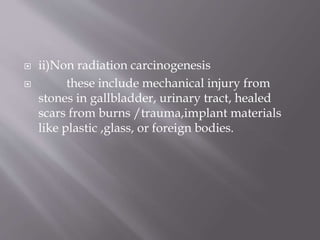
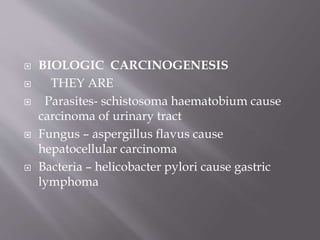
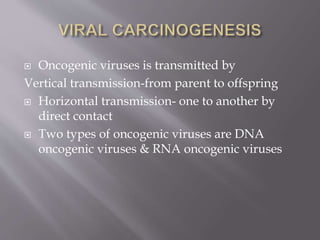
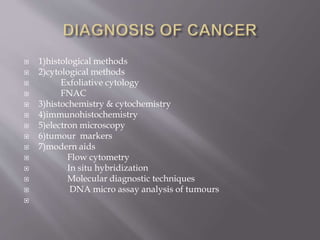
This document summarizes key concepts related to tumors and metastasis. It defines a tumor as abnormal cell proliferation. Metastasis occurs when tumor cells spread from the primary site to other parts of the body through routes like lymphatic or blood vessels. Common sites of metastasis include the liver, lungs, bones and brain. Carcinogens and genetic factors can cause carcinogenesis, the process of tumor formation. Grading and staging provide information on tumor characteristics and spread.