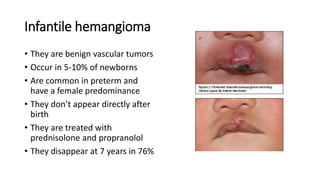
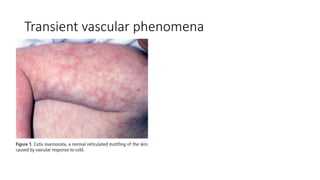
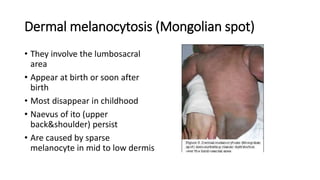
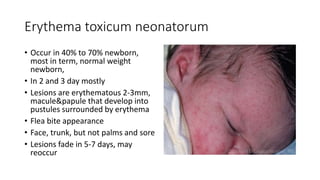
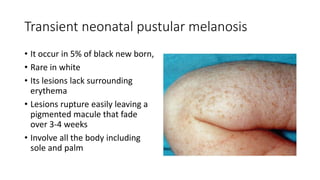
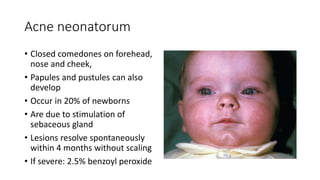
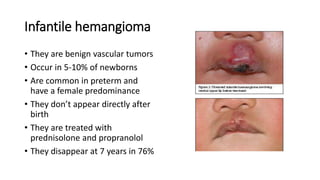
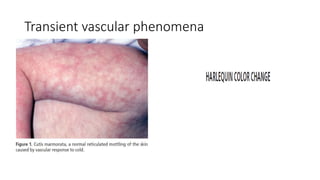
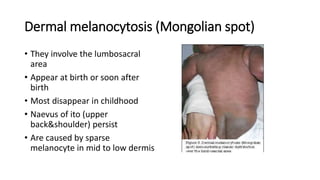
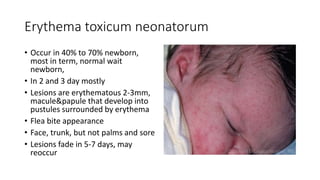
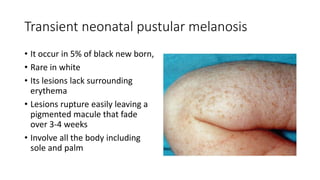
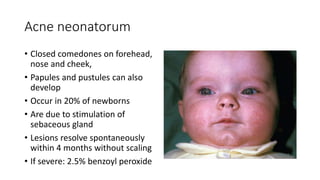
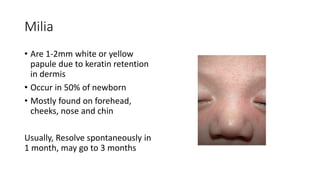
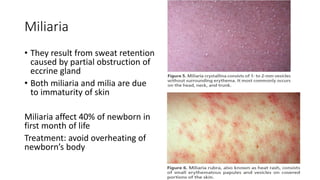
This document discusses common skin rashes that occur in neonates. It describes vascular lesions like infantile hemangiomas and pigmented lesions such as Mongolian spots. It also covers vesicopustular lesions including erythema toxicum neonatorum and acne neonatorum. Many of these rashes are transient and benign, but some may require treatment or workup. The document provides details on symptoms, prevalence, treatment and expected resolution time for various neonatal skin conditions.