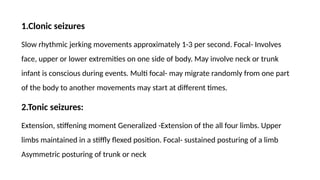
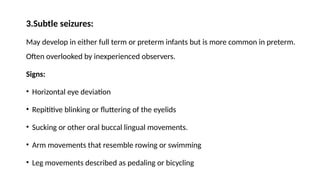
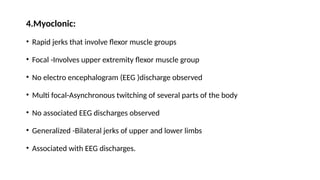
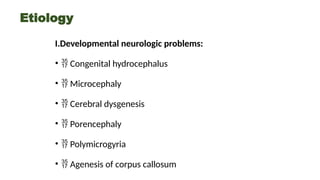
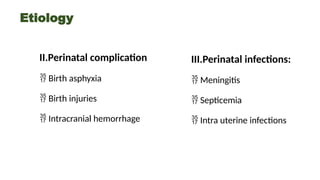
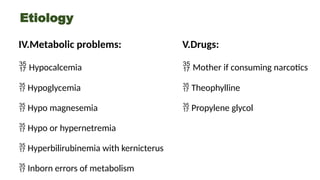
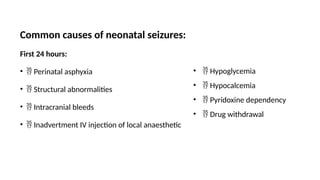
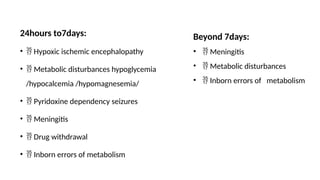
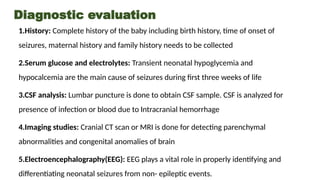
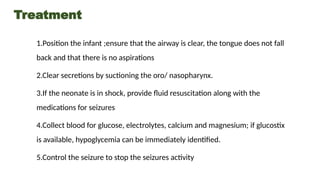
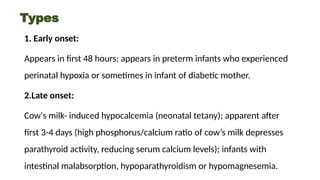
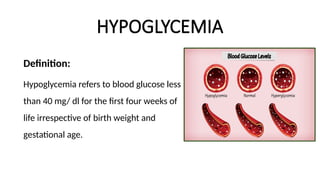
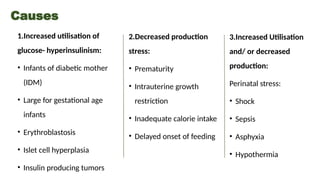
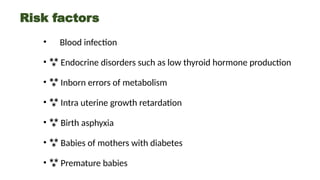
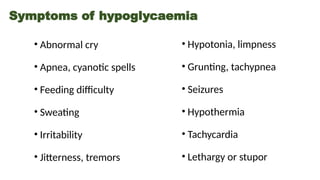
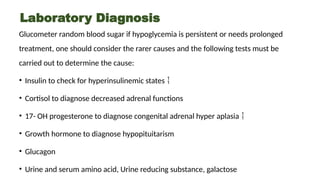
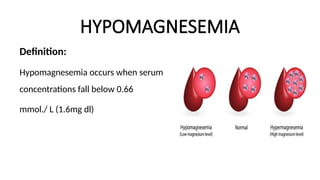
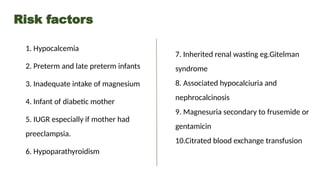
Neonatal seizures are categorized into four types: clonic, tonic, subtle, and myoclonic, with various etiologies including developmental issues, perinatal complications, infections, metabolic problems, and drug exposures. Diagnosis involves history-taking, serum tests, CSF analysis, imaging, and EEG, while treatment focuses on seizure activity control, airway management, and underlying causes. Common conditions associated with neonatal seizures include hypoglycemia, hypocalcemia, and hypomagnesemia, necessitating regular monitoring and management by healthcare providers.