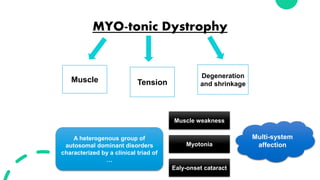
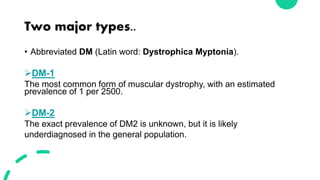
Myotonic muscular dystrophies are a group of inherited disorders characterized by muscle weakness and myotonia. There are two major types: DM1 and DM2. DM1 is caused by a CTG repeat expansion on chromosome 19 and is the most common type. DM2 is caused by a CCTG repeat expansion on chromosome 3. Both are dominantly inherited but only DM1 shows anticipation between generations. Symptoms range from late-onset weakness to congenital forms. Beyond muscle involvement, both types can affect multiple systems including the heart, eyes, gastrointestinal tract, and cognition. Management focuses on symptom control and multi-system screening due to the variable and progressive nature of the diseases.