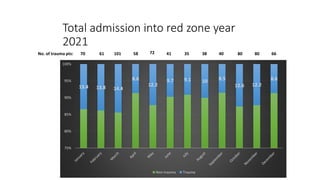
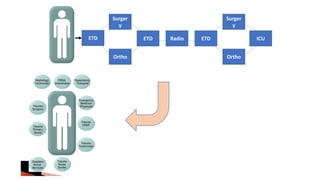
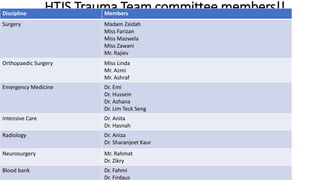
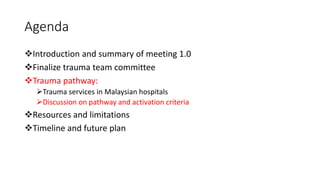
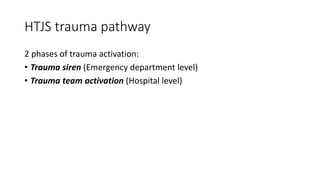
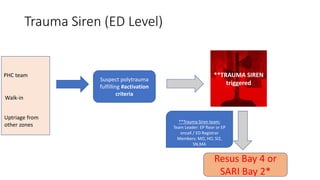
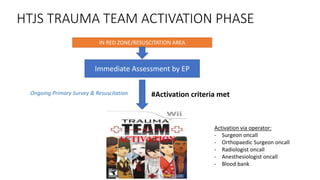
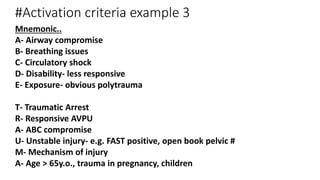
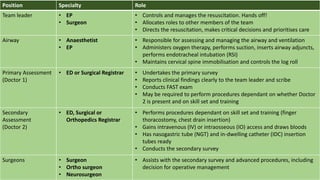
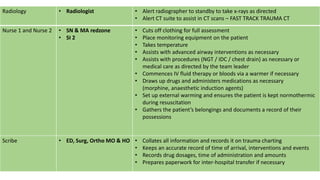
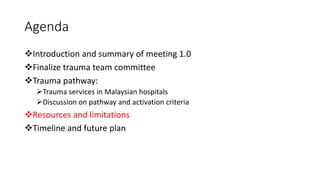
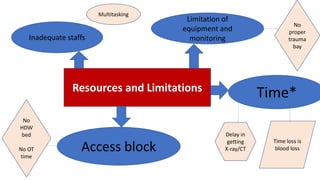
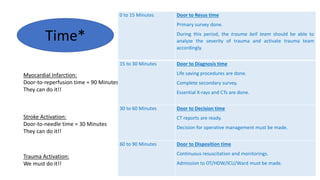
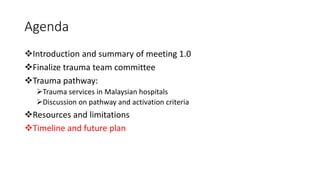
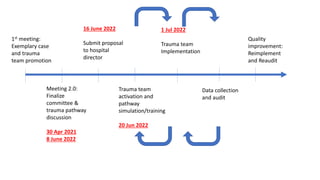
The multidisciplinary trauma team meeting held on June 8, 2022, focused on optimizing trauma services in Malaysian hospitals, finalizing the trauma team committee, and discussing trauma activation criteria and resources. The objectives of the trauma team include improving coordination in acute care, reducing intervention times for critical injuries, and ultimately enhancing survival rates for trauma patients. Key activation criteria for trauma team response were highlighted, emphasizing the importance of timely assessments and interventions during the trauma care process.