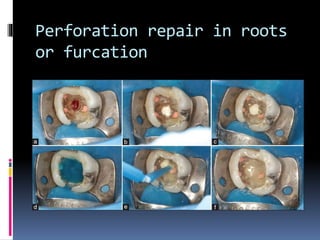
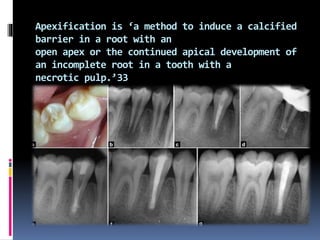
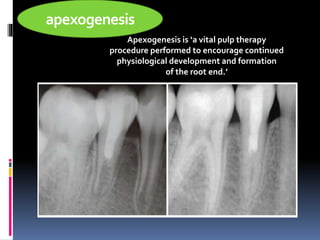
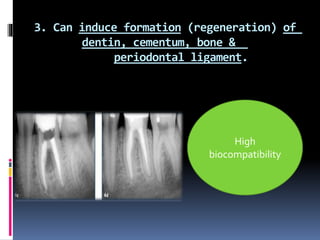
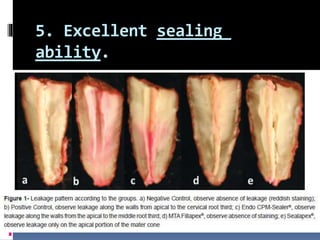
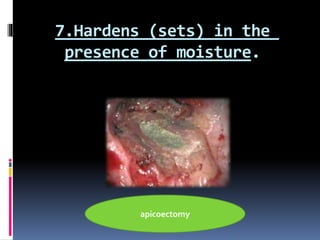
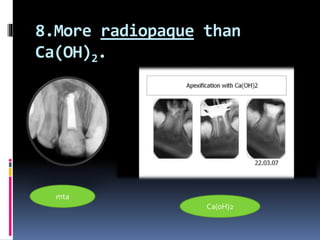
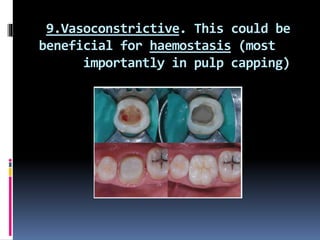
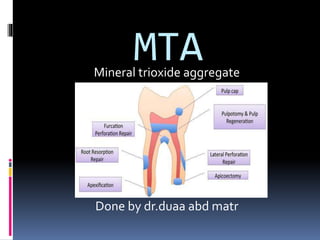
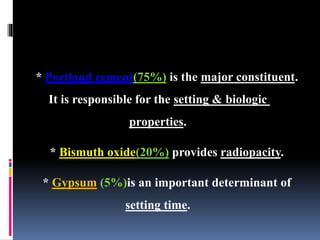
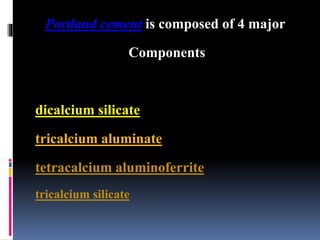
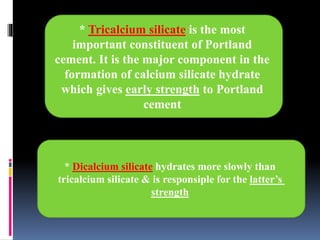
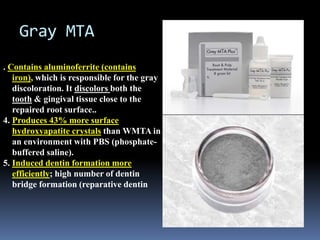
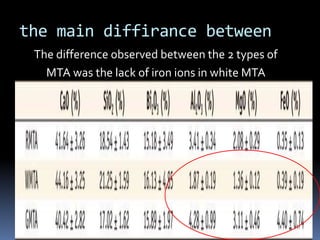
This document summarizes properties and clinical applications of mineral trioxide aggregate (MTA). MTA was introduced in 1993 and can be used for pulp capping, repair of root perforations, apexification, and as a root-end filling material. MTA sets in the presence of moisture and has antibacterial properties due to its high pH. It stimulates tissue regeneration and has good biocompatibility and sealing ability. Gray and white MTA are similar but white MTA lacks iron and is tooth-colored. MTA has advantages over other materials but also limitations such as a long setting time and difficult handling.

![Insertion: Ultrasonic-assisted condensation [the
ultrasonic vibration applied to endodontic
plugger(condenser)] is more efficient than hand
condensation in:
- the apical flowing of MTA (enable better flow).
- delaying bacterial leakage (enable better
adaptation).
- the production of denser MTA apical plug](https://image.slidesharecdn.com/random-150126153838-conversion-gate02/85/mta-17-320.jpg)