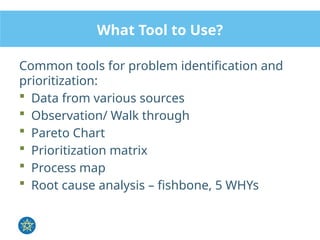
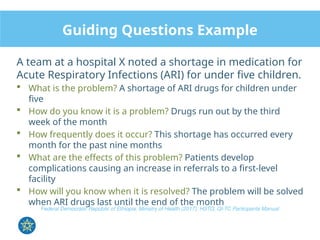
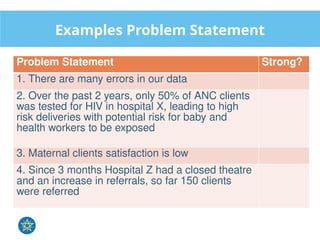
The document discusses strategies for identifying and prioritizing problems related to maternal mortality within healthcare facilities, emphasizing the need for effective problem statements and aim statements to guide quality improvement efforts. Participants engage in exercises that leverage quality dimensions, data analysis, and prioritization tools like the Pareto chart to determine focal areas for improvement. Ultimately, the document underscores the importance of structured approaches in addressing healthcare quality issues to enhance patient outcomes.