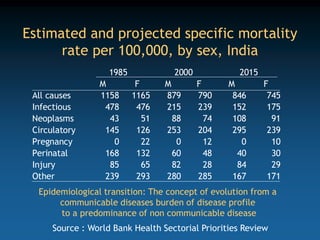
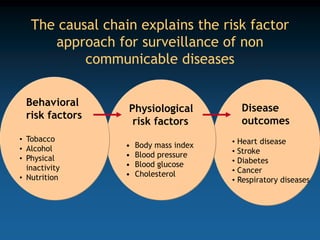
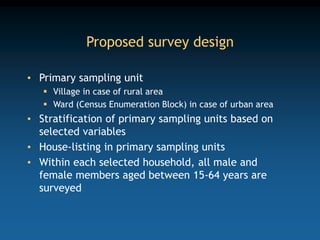
This document discusses surveillance of risk factors for non-communicable diseases (NCDs) in India. It describes the need for NCD risk factor surveillance given the increasing burden of NCDs. Surveillance of risk factors like tobacco use, alcohol consumption, obesity, diet, physical activity and blood glucose/cholesterol levels is recommended through periodic sample surveys. The role of district surveillance officers includes organizing such surveys involving collection of demographic, behavioral and biological data on NCD risk factors from the community. Ensuring valid and reliable surveillance methods is important to generate accurate data on trends and patterns of NCD risk factors.