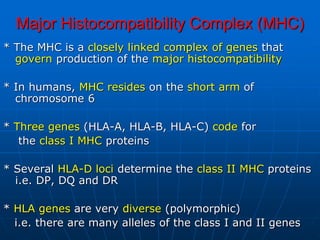
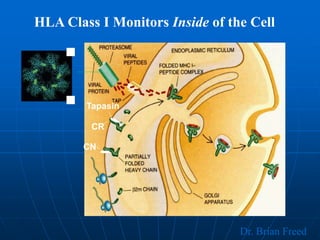
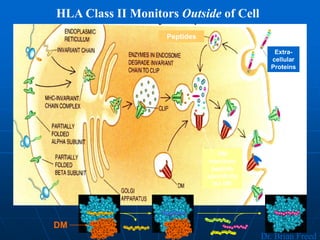
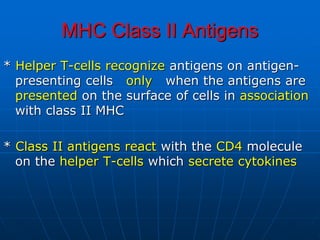
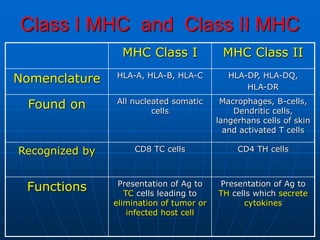
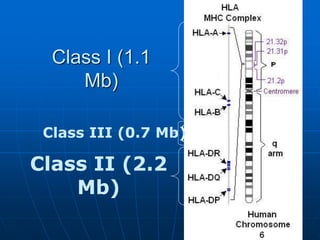
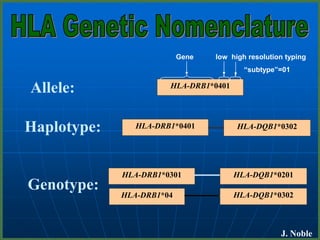
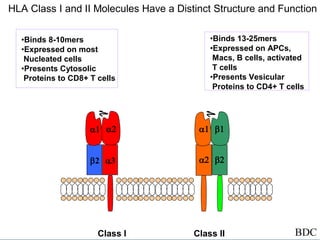
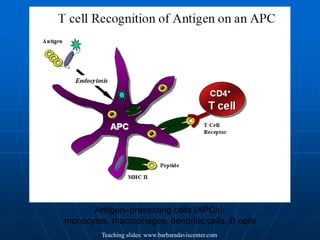
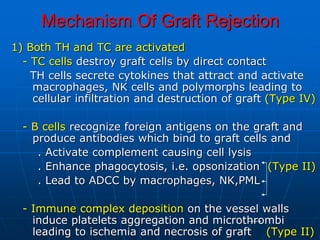
The major histocompatibility complex (MHC) genes code for cell surface proteins that present antigens to T cells. In humans, MHC genes are located on chromosome 6 and are highly polymorphic. There are three main MHC classes - class I presents intracellular antigens to CD8+ T cells, class II presents extracellular antigens to CD4+ T cells, and class III encodes complement and cytokine proteins. MHC matching is important for transplant acceptance, as mismatches can lead to graft rejection through cellular and antibody-mediated immune responses.