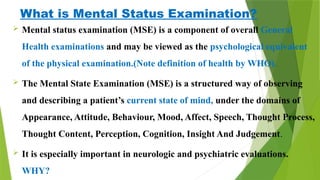
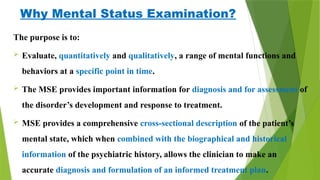
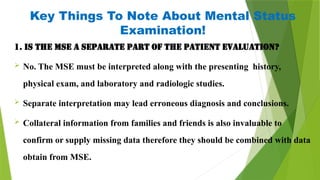
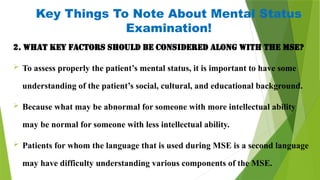
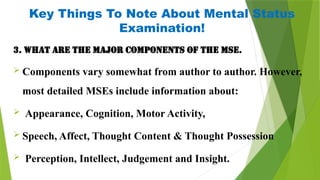
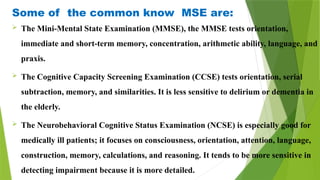
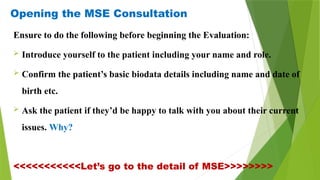
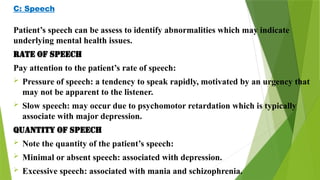
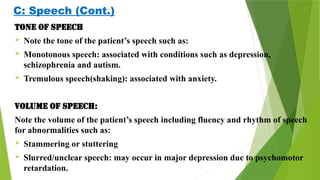
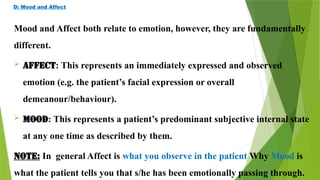
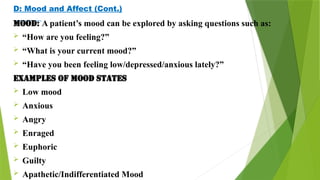
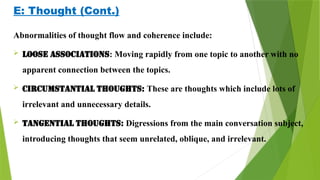
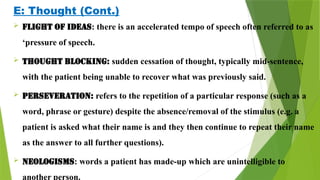
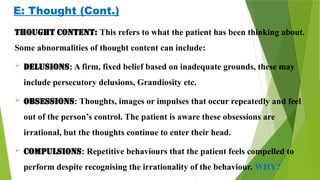
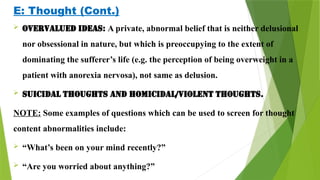
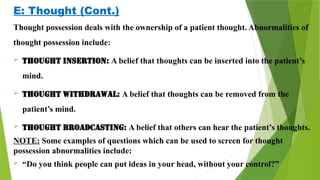
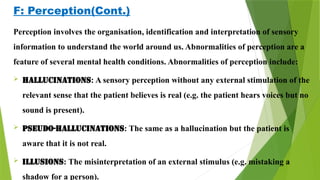
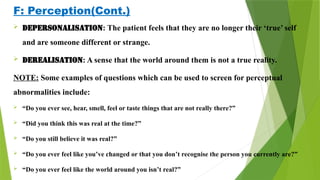
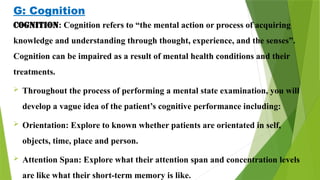
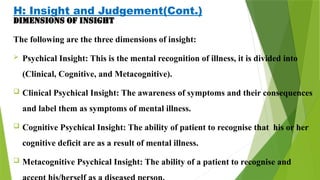
The document presents a comprehensive overview of the Mental Status Examination (MSE), detailing its significance in evaluating a patient's current mental state through various domains such as appearance, behavior, mood, and cognition. It emphasizes that the MSE is integral to overall patient evaluation and must be interpreted in conjunction with additional clinical data. The document also outlines key components and observations necessary for assessing mental health, underscoring the importance of understanding a patient's background and the collaborative nature of the assessment process.