1) People with mental illness are more susceptible to poor physical health due to unhealthy lifestyles, medications, and barriers to healthcare access.
2) Physical activity can improve mental health - studies show it reduces depressive symptoms and has similar effects as cognitive therapy.
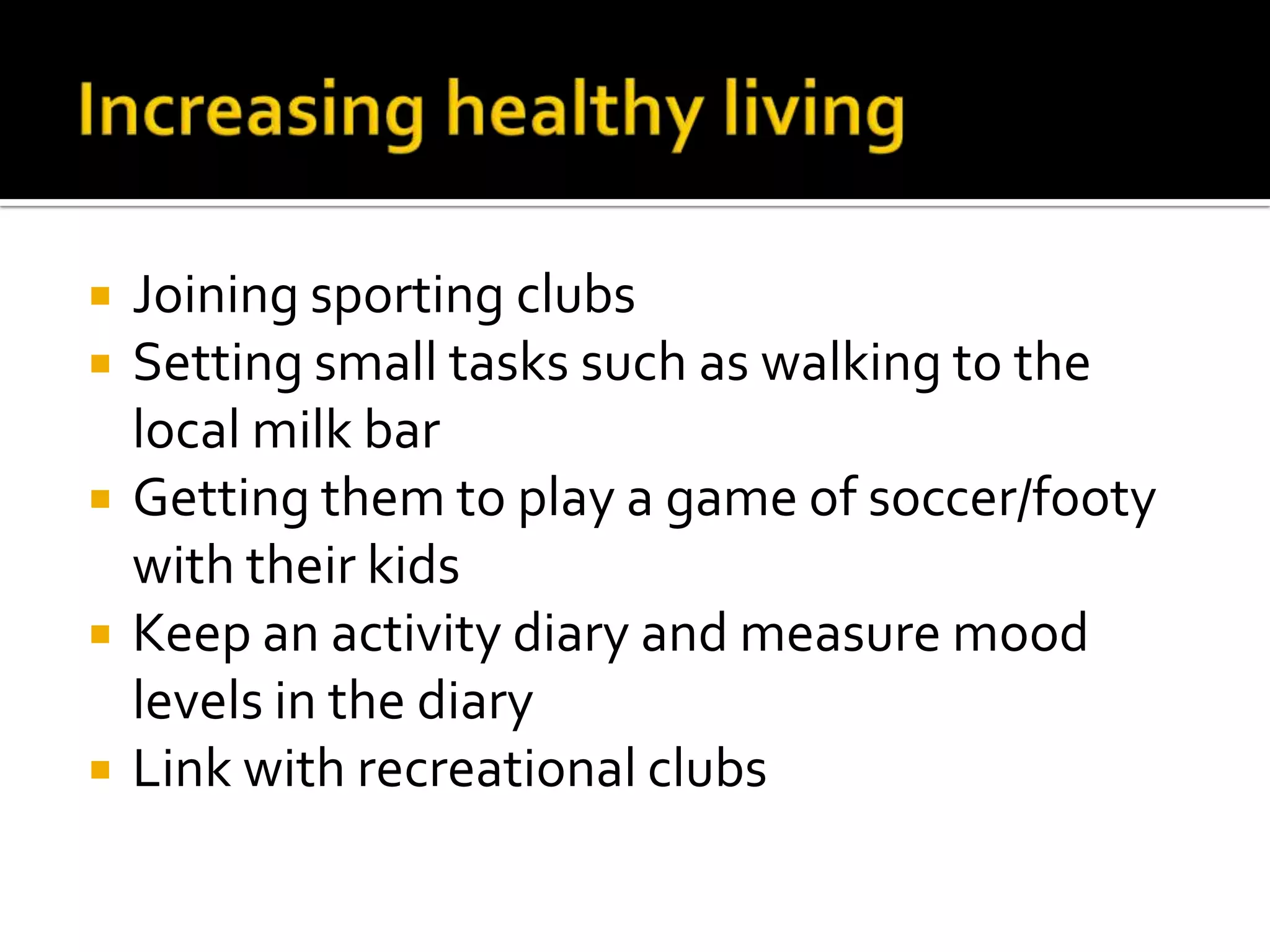
3) Improving physical health for those with mental illness requires a multi-pronged approach, including discussing physical health at appointments, flexible assessments, ensuring follow-up care, and partnerships between patients, families, and clinicians.