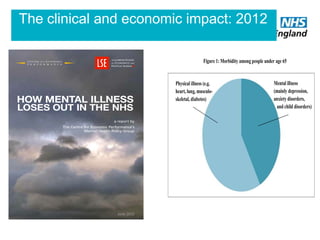
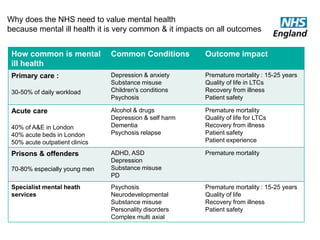
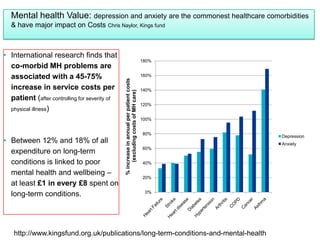
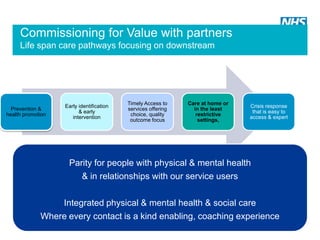
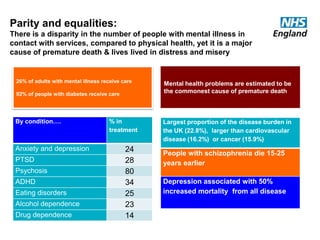
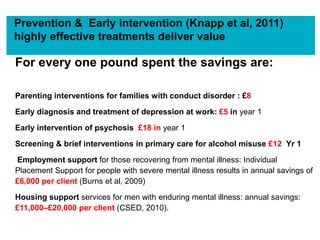
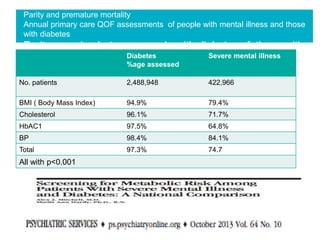
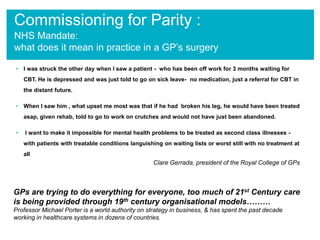
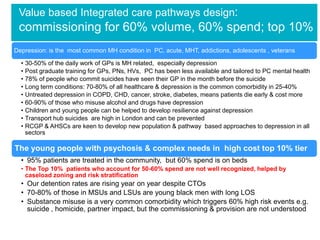
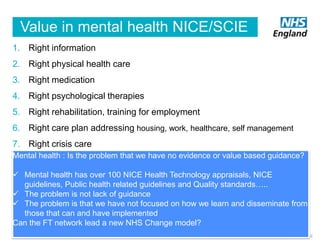
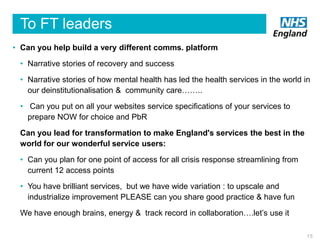
This document discusses valuing mental health in the NHS. It notes that mental health issues are very common, impacting outcomes and costs. Parity is needed between treating mental and physical health issues. The document provides statistics on the prevalence and impact of various mental health conditions. It discusses how mental health issues increase costs for long term physical conditions. Integrated care pathways and prevention/early intervention can deliver cost savings. More work is needed to achieve parity, such as ensuring equal access to assessments and treatments for mental and physical issues. The NHS aims to support value-based commissioning through various programs and specifications. FT networks are asked to help transform services by sharing best practices to improve access, integration and outcomes nationwide.