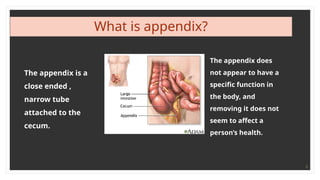
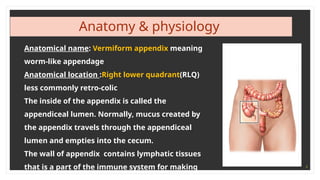
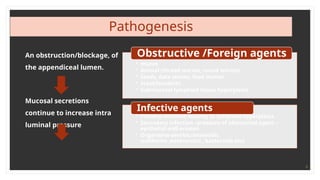
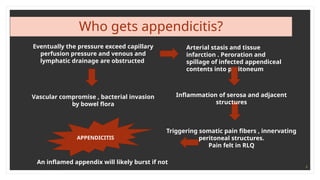
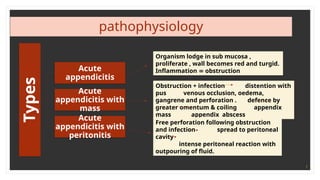
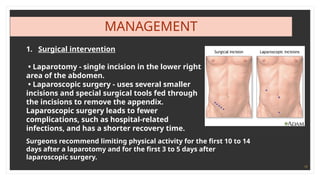
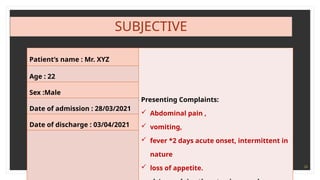
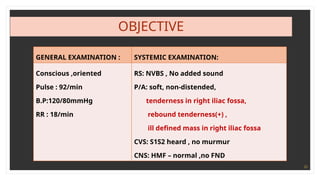
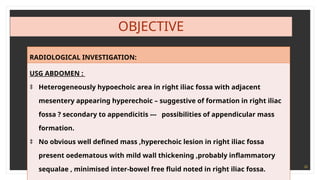
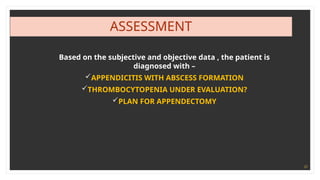
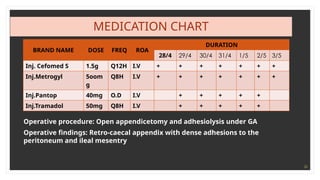
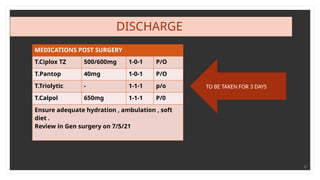
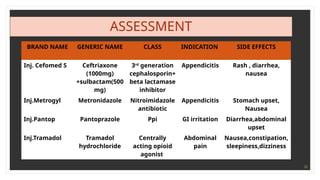
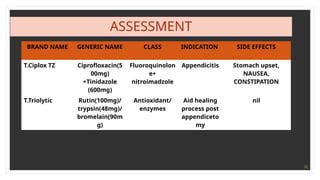
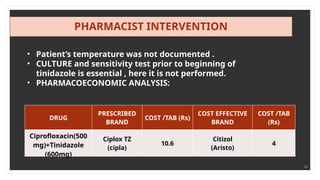
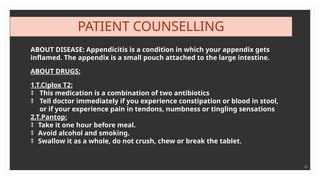
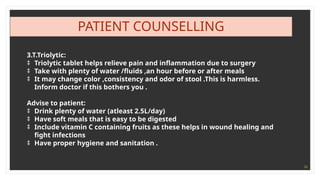
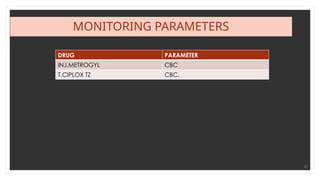
Appendicitis is an inflammation of the appendix, often requiring emergency surgery due to potential complications like a burst appendix. Symptoms include sudden abdominal pain, nausea, and fever, and diagnosis can typically be made through medical history and physical exams. Treatment includes surgical intervention, antibiotics, and dietary guidelines post-surgery to ensure recovery.