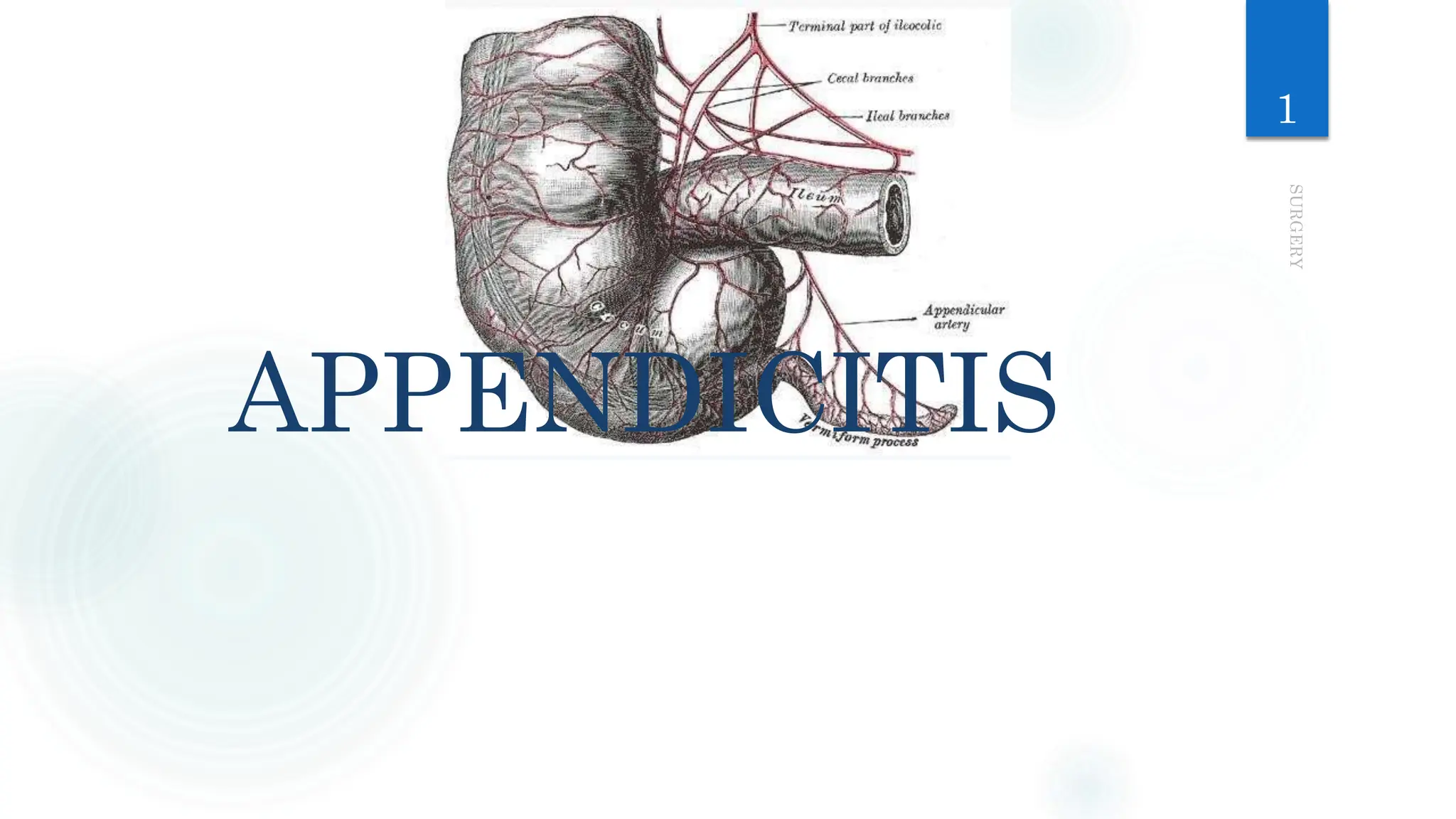
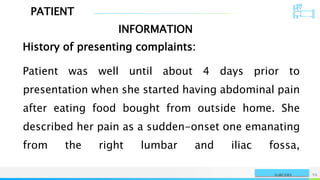
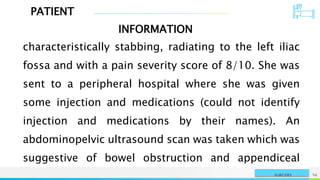
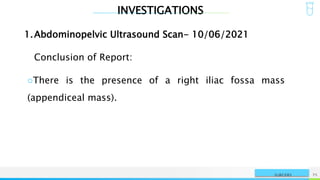
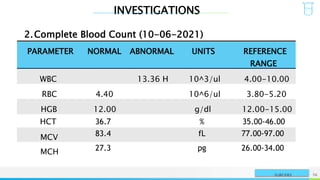
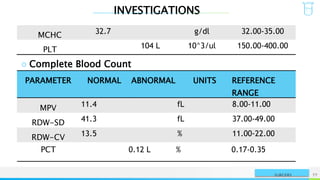
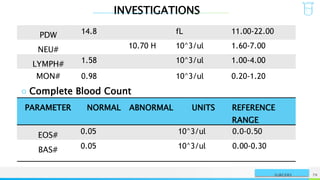
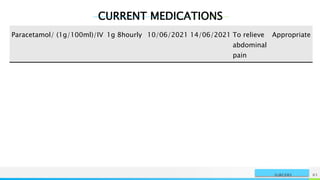
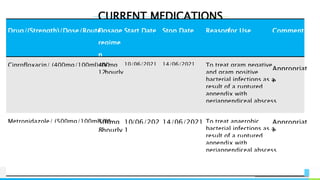
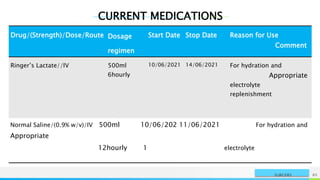
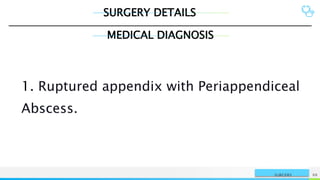
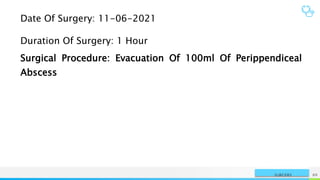
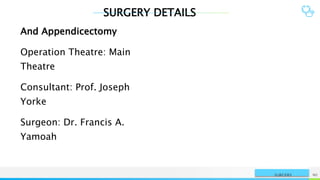
The patient, a 15-year-old female, presented with abdominal pain and was found to have a ruptured appendix and periappendiceal abscess based on ultrasound findings. She underwent an appendectomy and drainage of the abscess. Her postoperative recovery was uneventful and she was discharged after one week with oral antibiotics.

![SYMPTOMS AND SIGNS
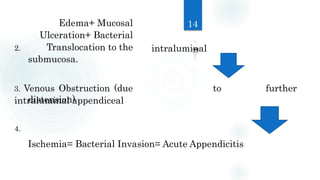
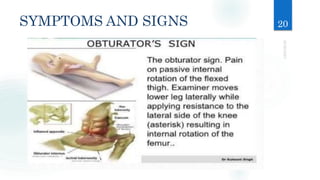
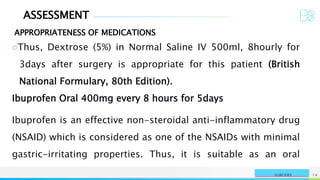
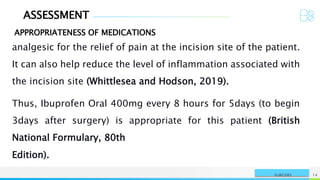
4. Pain caused by passive internal rotation of the flexed thigh
5. Low-grade fever (rectal temperature
37.7 to 38.3° C [100 to
(obturator sign) .
101° F]) is common.](https://image.slidesharecdn.com/apx-240212212425-2c95f792/85/Appendicitis-Presentation-By-Danso-Jephthah-Kwasi-29-320.jpg)

![DIAGNOSIS
Laparoscopy canbe used for
diagnosis definitive treatment of
appendicitis; especially helpful in
women with lower abdominal pain
of unclear etiology.
Laboratory studies typically show
leukocytosis (12,000 to 15,000/mcL [12.00 to 15.00 ×
109/L]), but this finding is highly variable.
27
as well as
it may be](https://image.slidesharecdn.com/apx-240212212425-2c95f792/85/Appendicitis-Presentation-By-Danso-Jephthah-Kwasi-41-320.jpg)

























![REFERENCES
SURGERY NAME OR LOGO 165
Gahart B.L. et al (2018), Gahart's 2018 Intravenous Medications: A
Handbook for Nurses and Health Professionals (34th Edition)
Elsevier Inc. London, United Kingdom. Pages 445-447.
Tonog P., Lakhkar A.D., Normal Saline. [Updated 2020 May 24]. In:
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing;
2020 Jan-. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK545210/.](https://image.slidesharecdn.com/apx-240212212425-2c95f792/85/Appendicitis-Presentation-By-Danso-Jephthah-Kwasi-165-320.jpg)