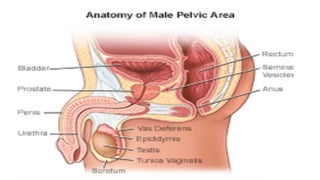
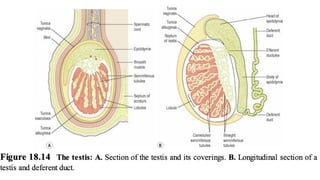
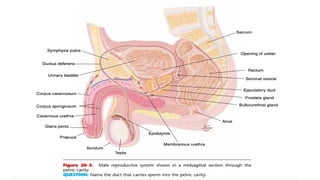
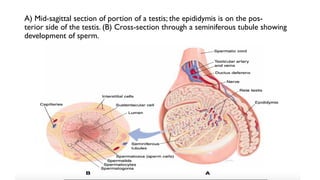
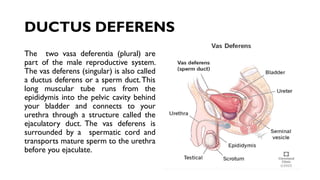
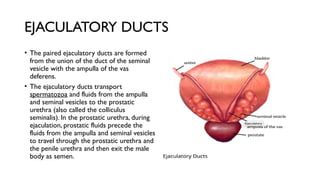
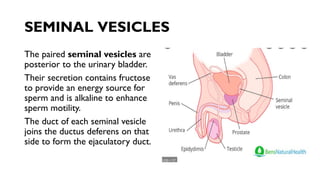
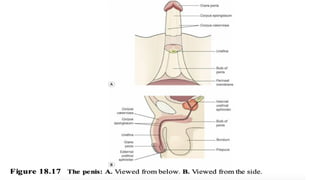
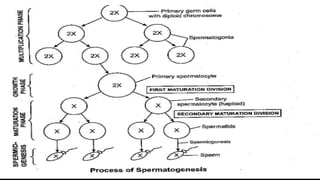
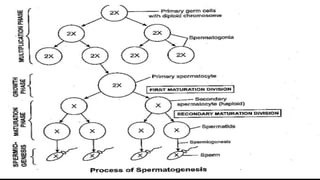
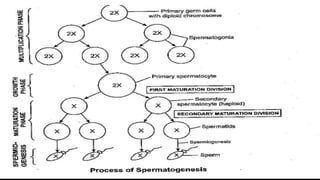
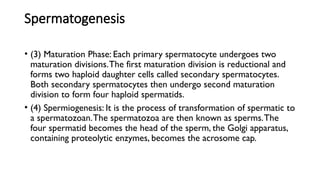
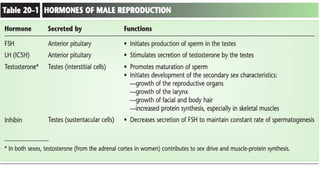
The document provides an overview of male reproductive anatomy and physiology, detailing the structure and function of various components such as the testes, scrotum, epididymis, ductus deferens, ejaculatory ducts, seminal vesicles, prostate gland, and bulbourethral glands. It explains the processes of sperm production (spermatogenesis) and the composition of semen, highlighting the importance of temperature regulation and hormonal influences. Additionally, it describes the role of different glands in semen formation and the pathway of sperm from the testes to ejaculation.