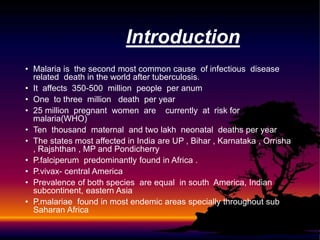
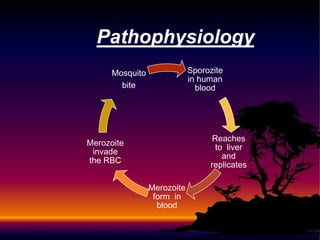
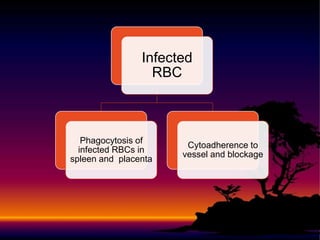
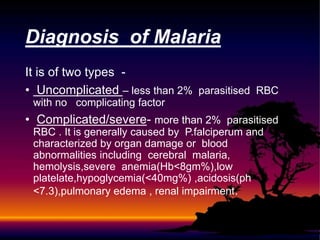
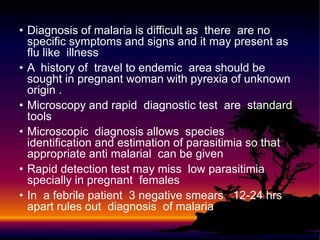
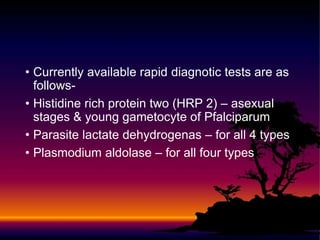
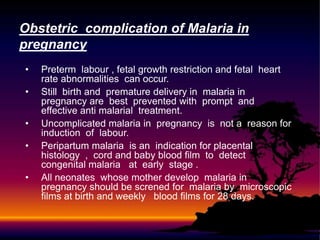
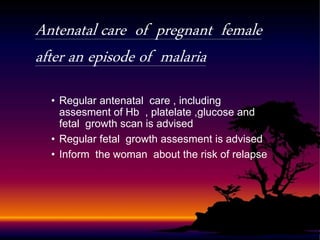
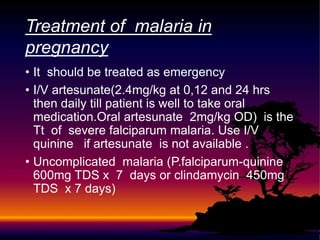
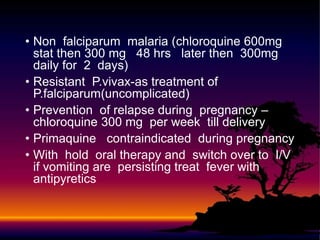
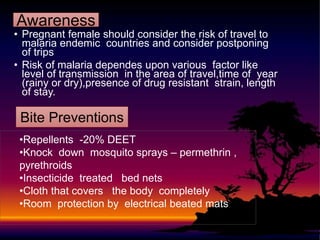
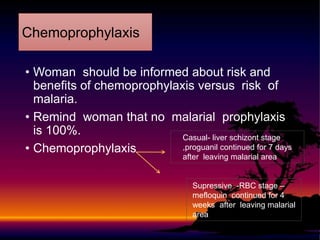
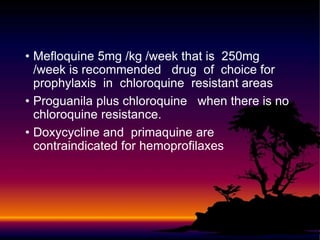
Malaria in pregnancy poses significant risks to both mother and baby. It can cause complications including preterm labor, low birth weight, and maternal or neonatal death. Pregnant women living in parts of Africa, Asia, and South America are most at risk. Diagnosis involves blood smears or rapid tests to detect the plasmodium parasites. Treatment depends on the severity of the case and parasite species, but prompt effective treatment is important to prevent poor outcomes. Prevention strategies for at-risk pregnant women include antimalarial chemoprophylaxis, insecticide-treated bed nets, and insect repellents.