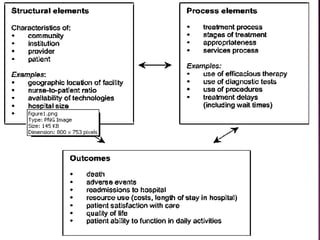
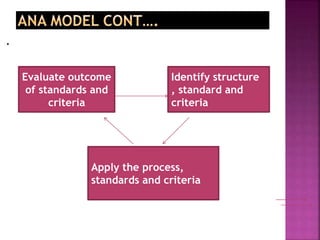
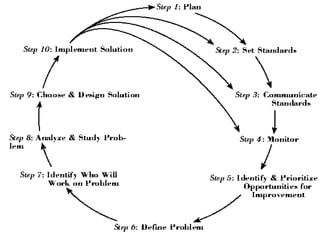
The document discusses quality assurance in healthcare. It defines quality assurance and provides definitions from various sources. It describes models of quality assurance including the Donabedian model of structure, process and outcomes. The document outlines the goals and importance of quality assurance in healthcare delivery as well as challenges in implementing quality assurance programs. It discusses general and specific approaches to quality assurance and monitoring quality of care.