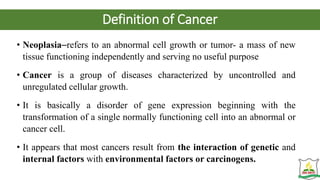
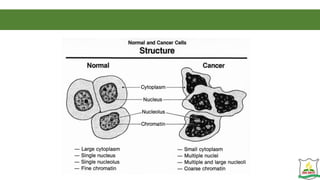
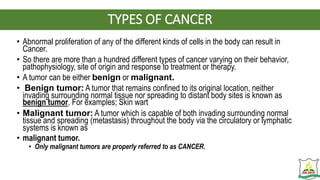
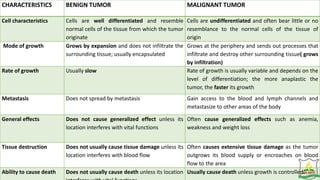
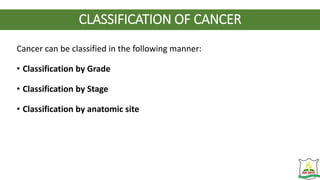
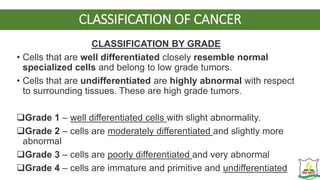
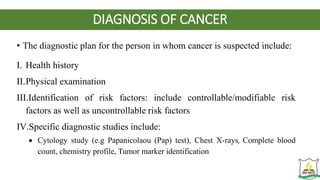
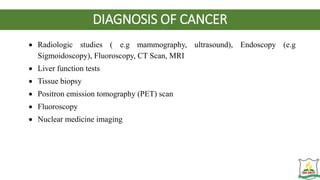
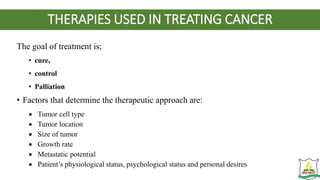
This document provides an overview of oncology and cancer. It begins by defining key terms like oncology and describing the characteristics of normal cells. It then discusses how cancer develops, defining cancer and describing the pathophysiology and carcinogenesis. It differentiates between benign and malignant tumors and identifies various carcinogens. The document continues by describing the classification, diagnosis, symptoms and treatment of cancer. It provides information on the nursing role in various cancer treatment modalities.

![RADIATION THERAPY
• Radiation therapy is the use of ionizing radiation to interrupt cellular growth.
• It is also used to control malignant disease when a tumour cannot be removed
surgically or when local nodal metastasis is present or it can be used
prophylactically to prevent leukemic infiltration to the brain or spinal cord.
• Radiation therapy may be used to cure the cancer, as in Hodgkin disease,
testicular seminomas, thyroid carcinomas, localized cancers of the head and
neck.
• There are two types of ionizing radiation:
• electromagnetic rays (x-rays and gamma rays) and
• particles (electrons [beta particles], protons, neutrons and alpha particles).](https://image.slidesharecdn.com/oncology-231022003926-30426af6/85/ONCOLOGY-pptx-43-320.jpg)