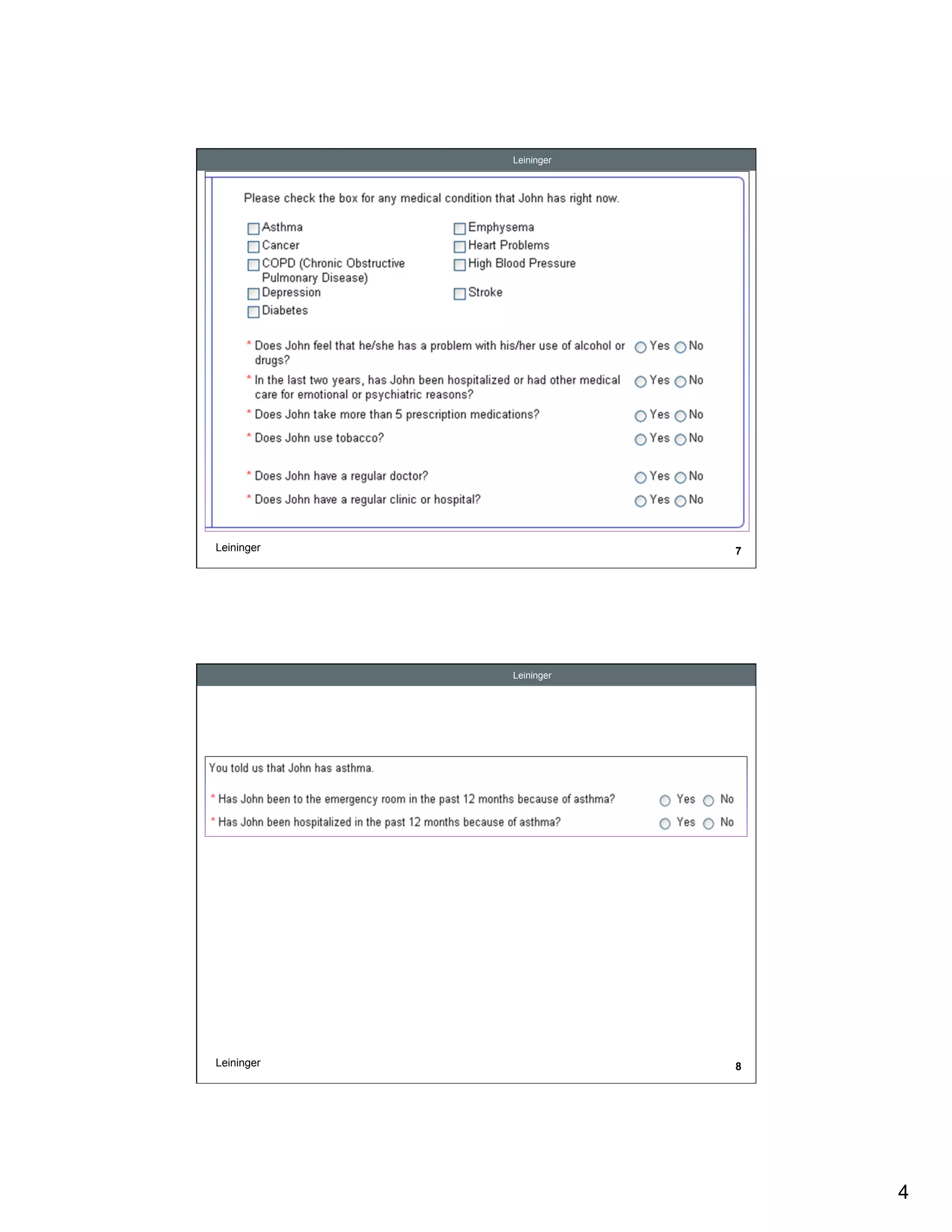
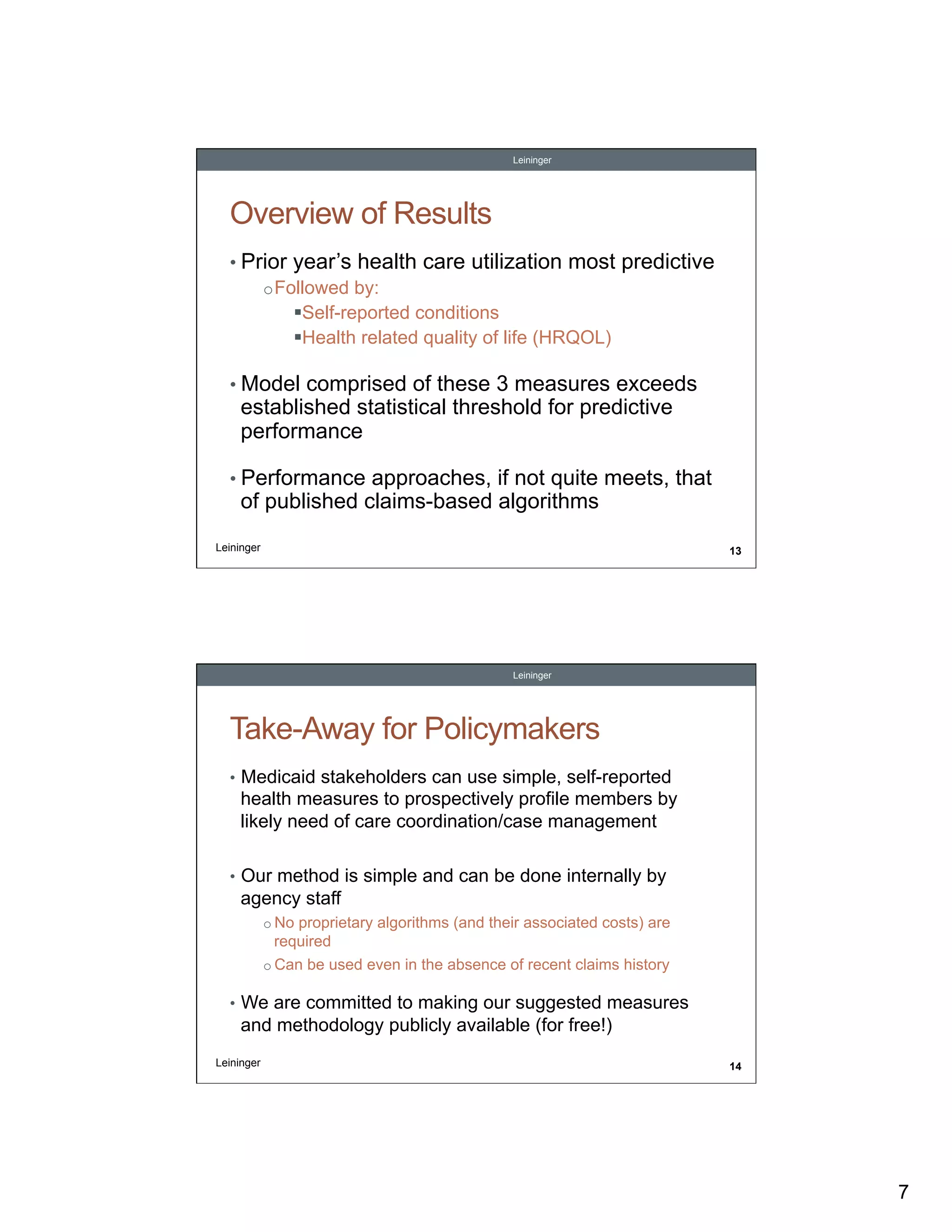
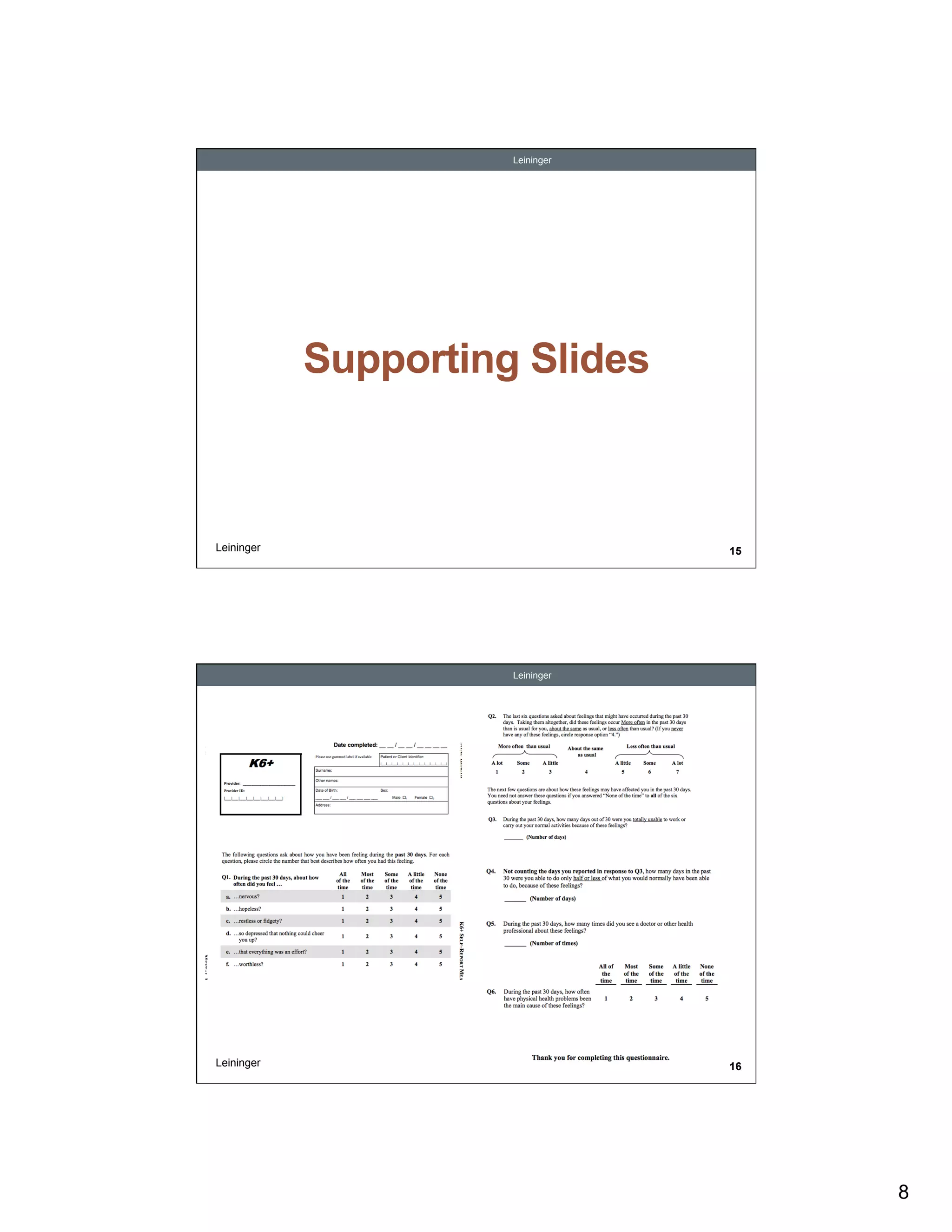
This document discusses prospectively identifying Medicaid-eligible adults who have high health care needs. It summarizes a study that tested whether self-reported health measures could serve as an alternative to claims data for predicting high-need individuals. The study found that measures of prior health care utilization, self-reported conditions, and health-related quality of life were predictive of outcomes like inpatient visits and high costs. It concludes that Medicaid agencies can use simple self-reported information to identify members for care coordination programs, without needing proprietary algorithms or claims histories.