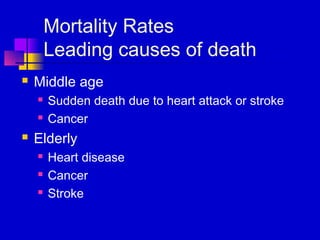
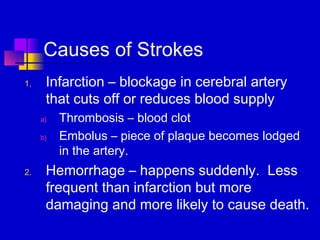
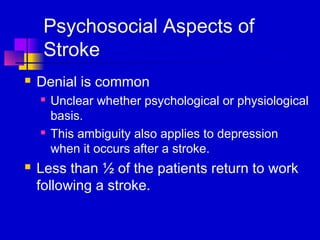
The document discusses leading causes of death across the lifespan, including congenital abnormalities and SIDS for infants under 1, accidents for children over 1, and heart disease, cancer, and stroke for adults and the elderly. It also discusses gender differences in mortality, with women living longer than men on average due to riskier behaviors and occupations among men. Finally, it covers heart disease, hypertension, and stroke in more detail, outlining symptoms, risk factors, treatment options, and effects.