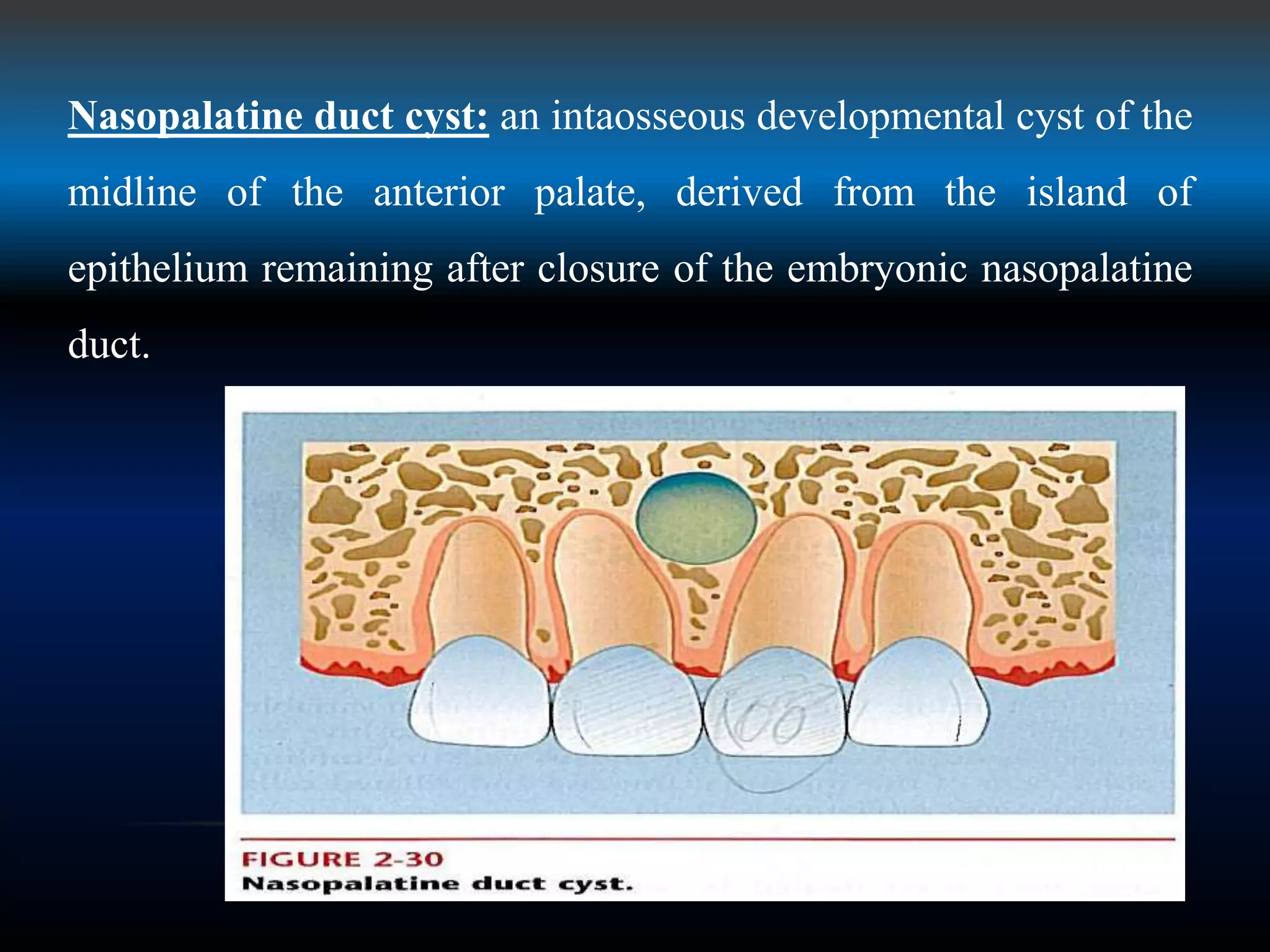
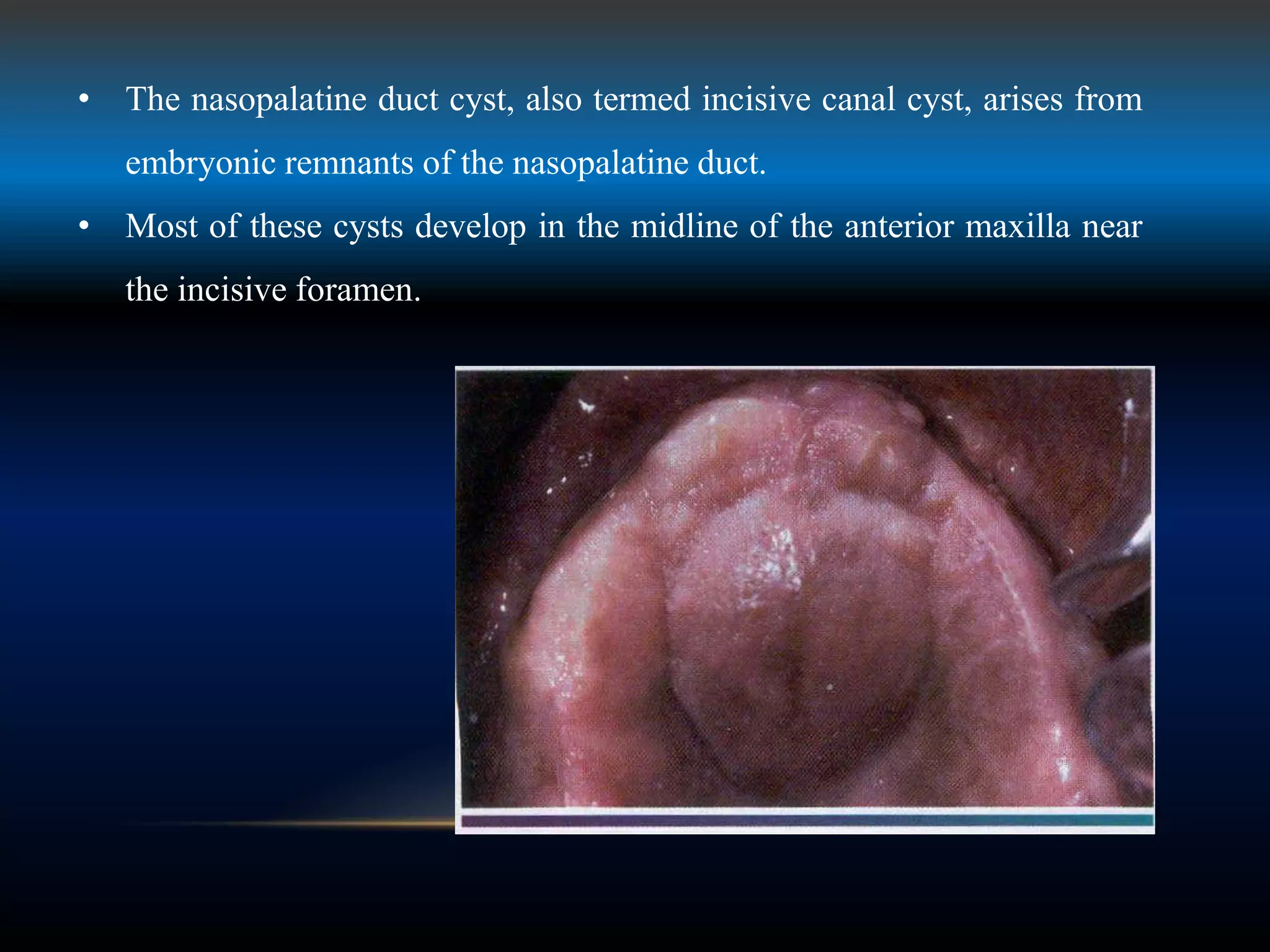
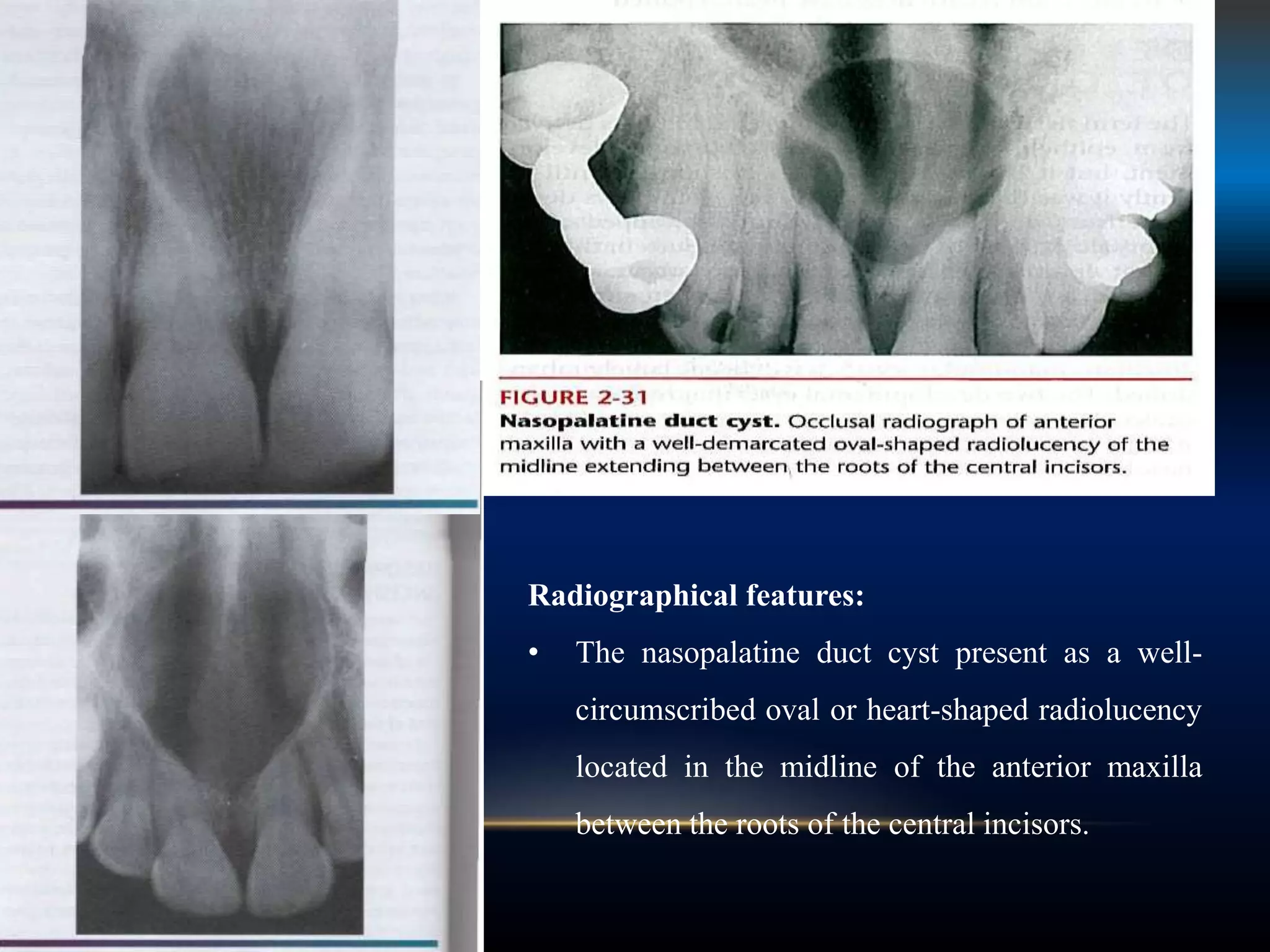
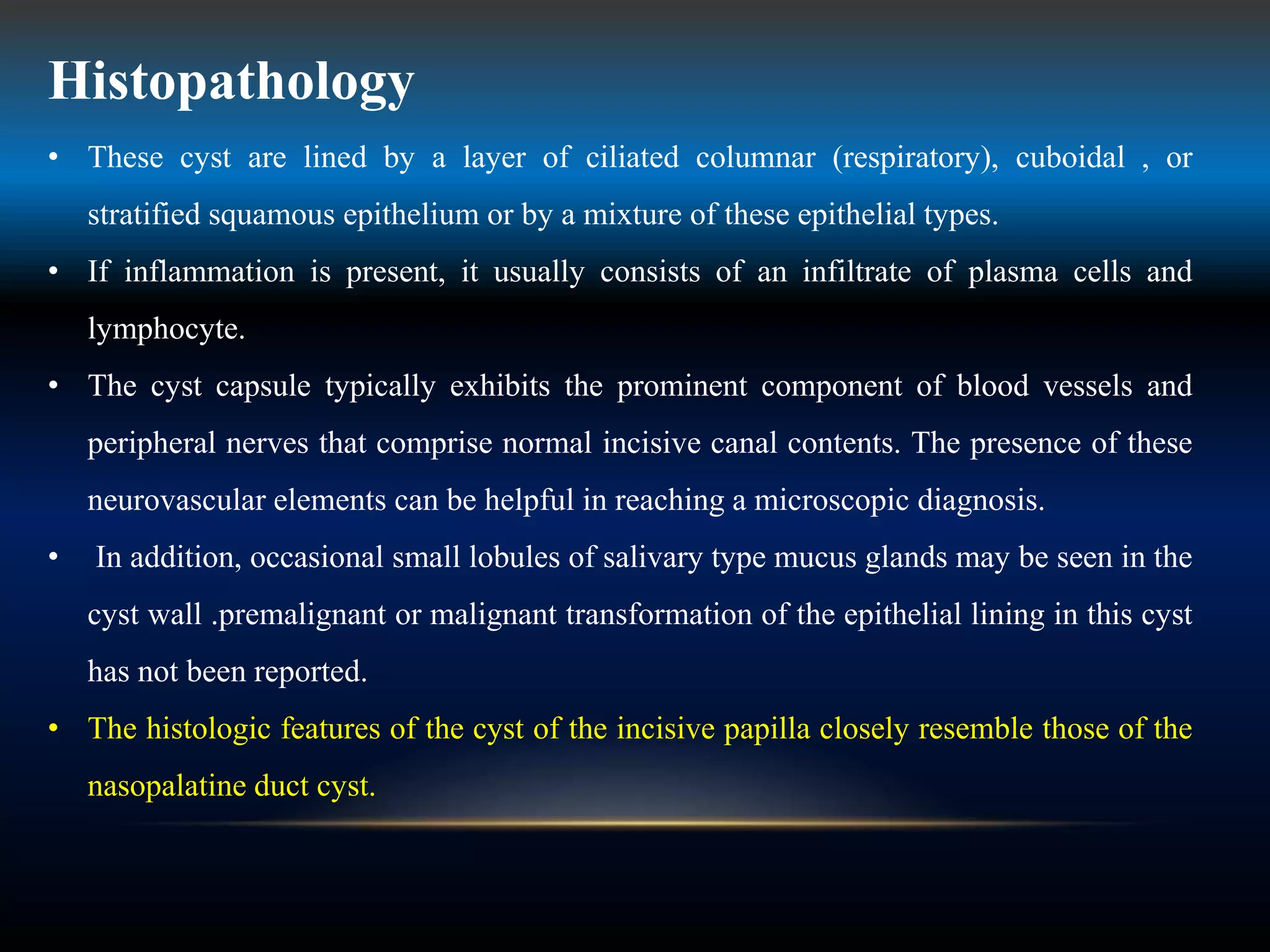
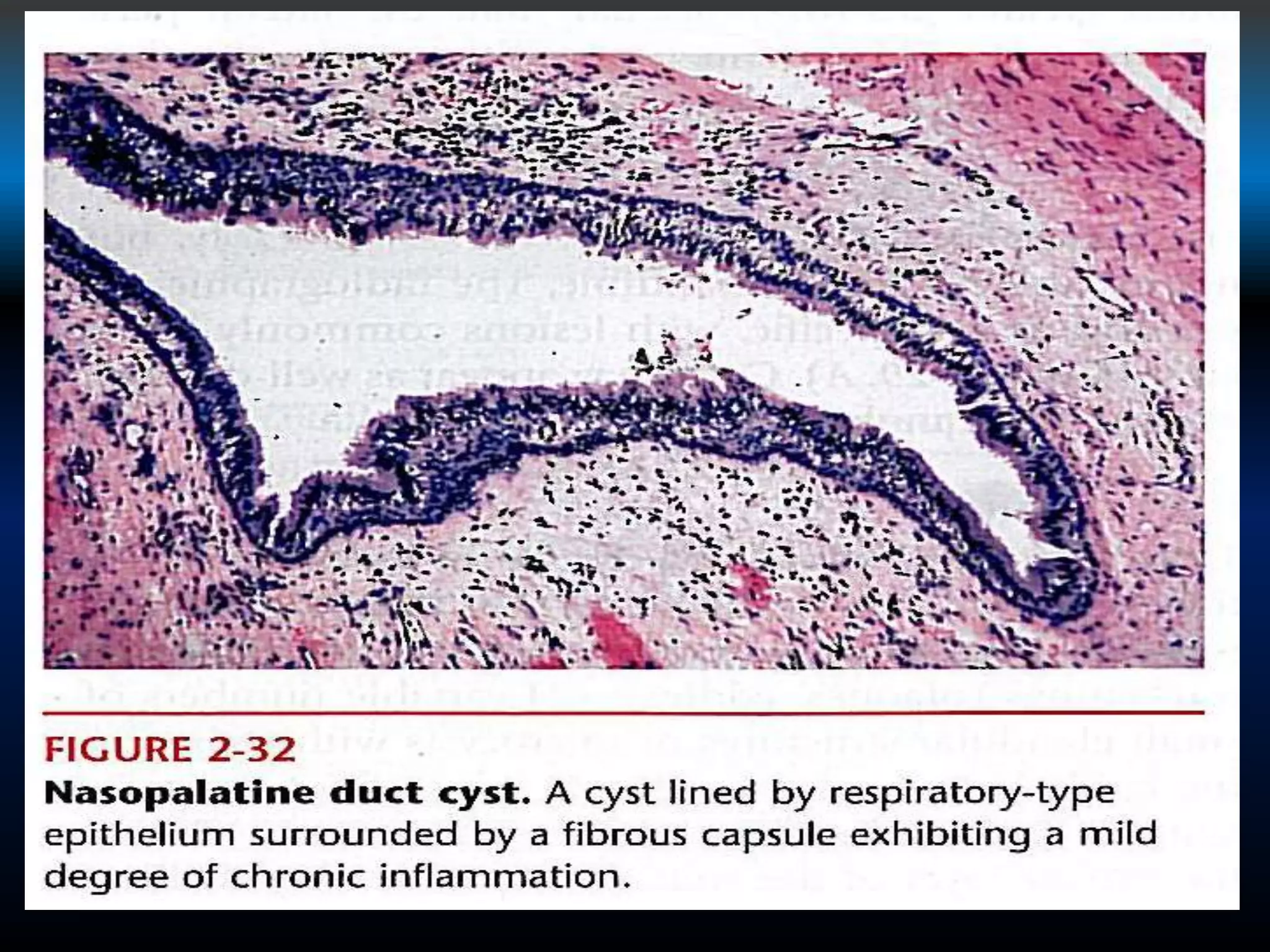
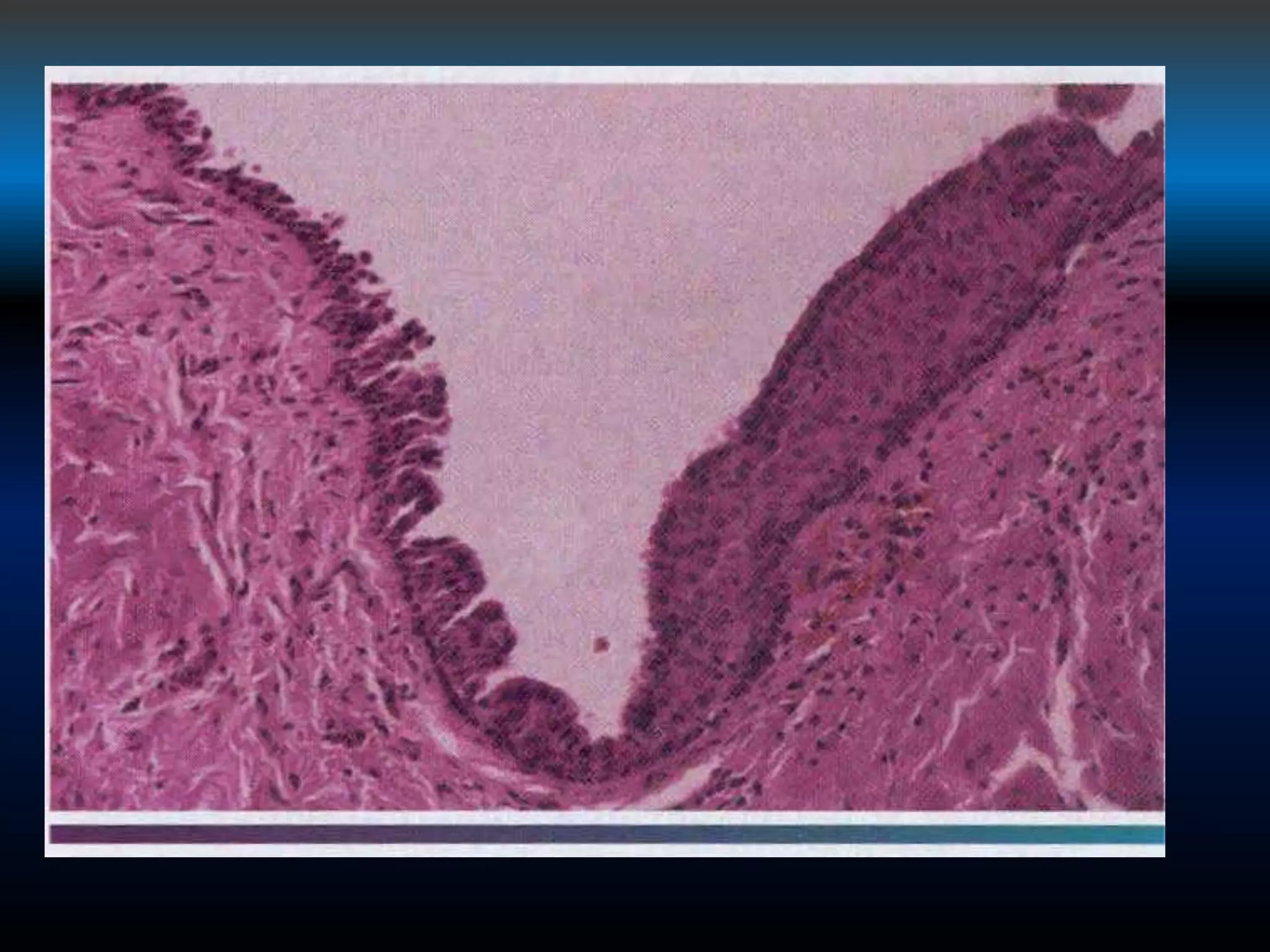
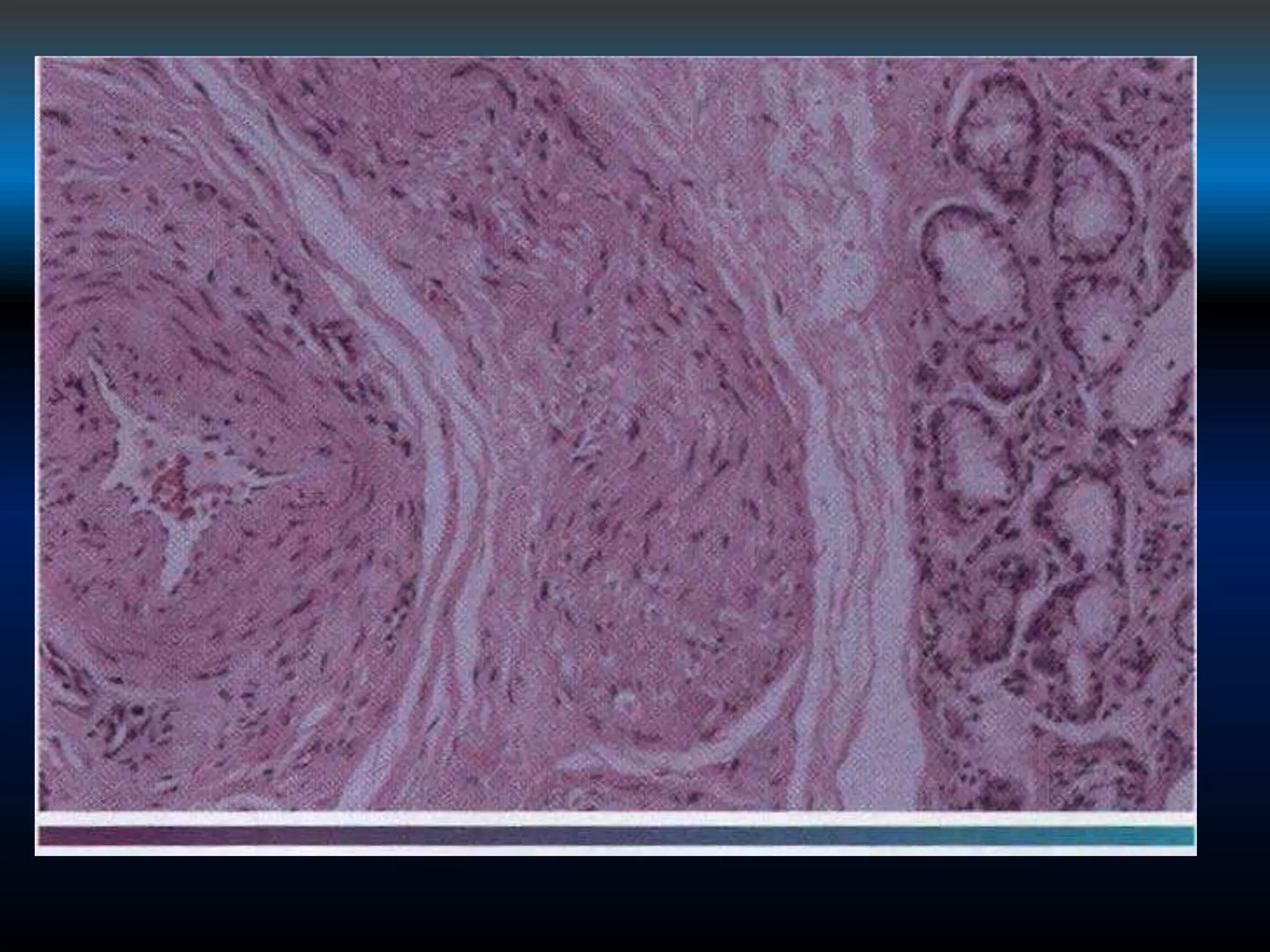
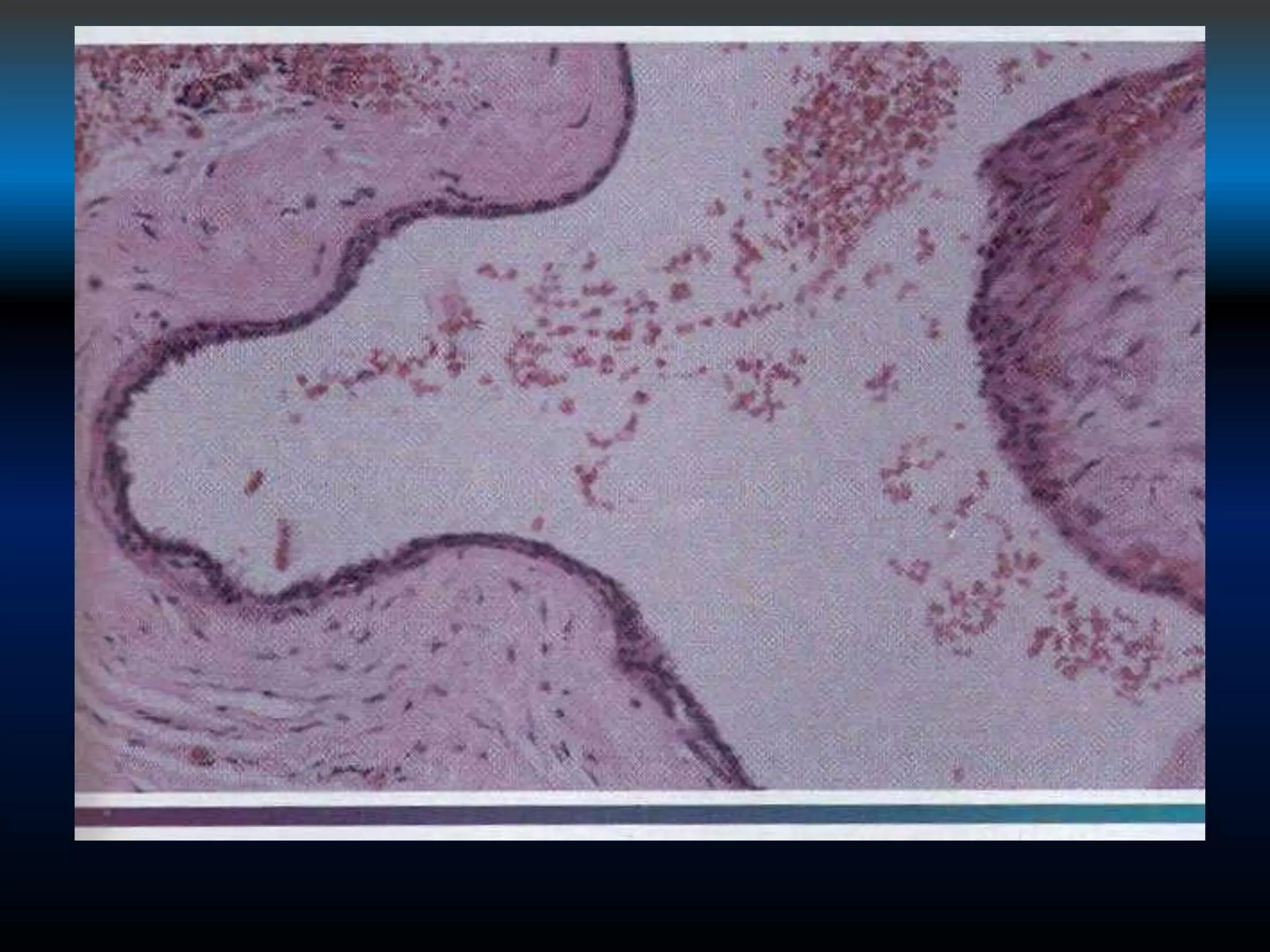
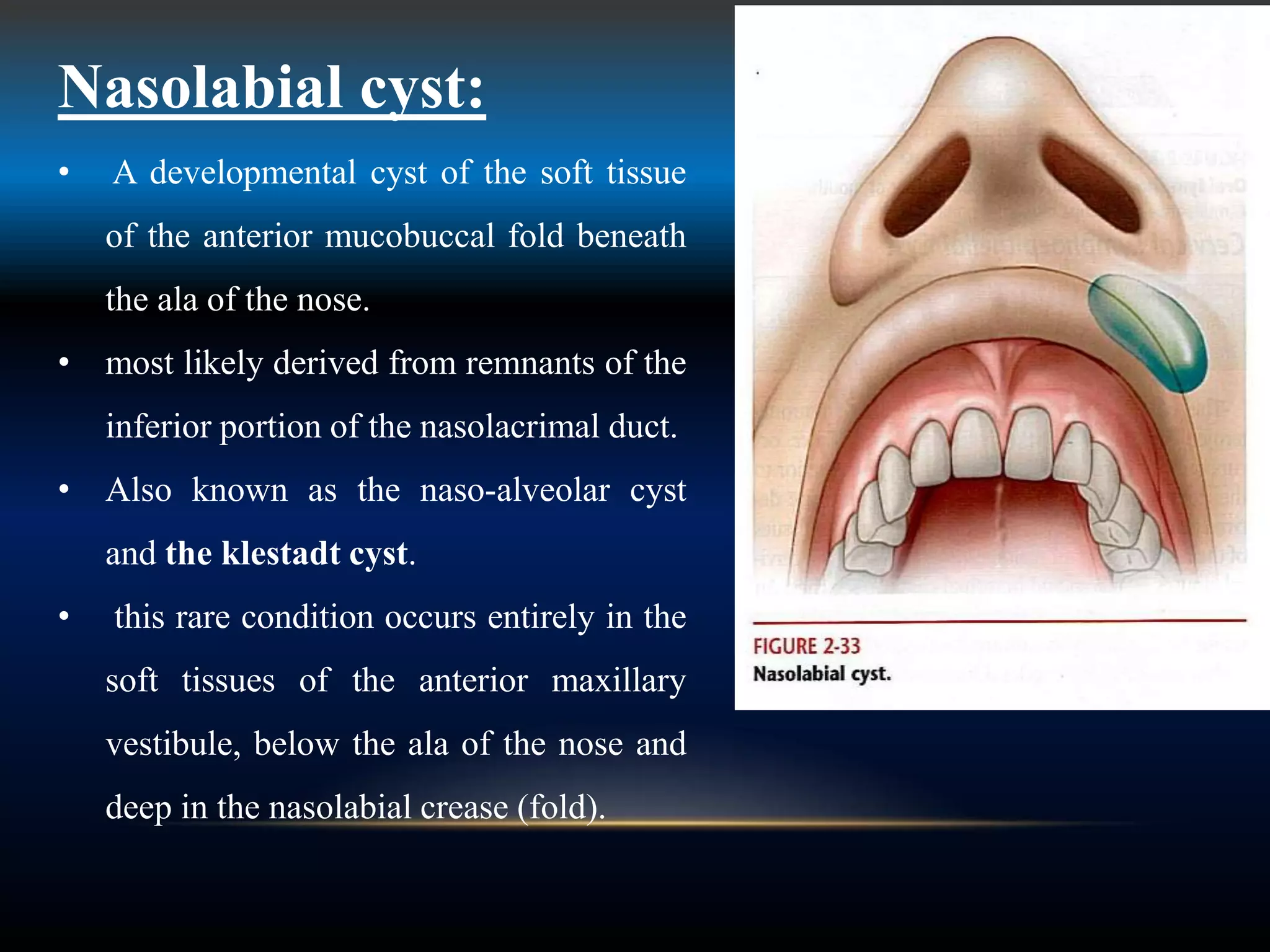
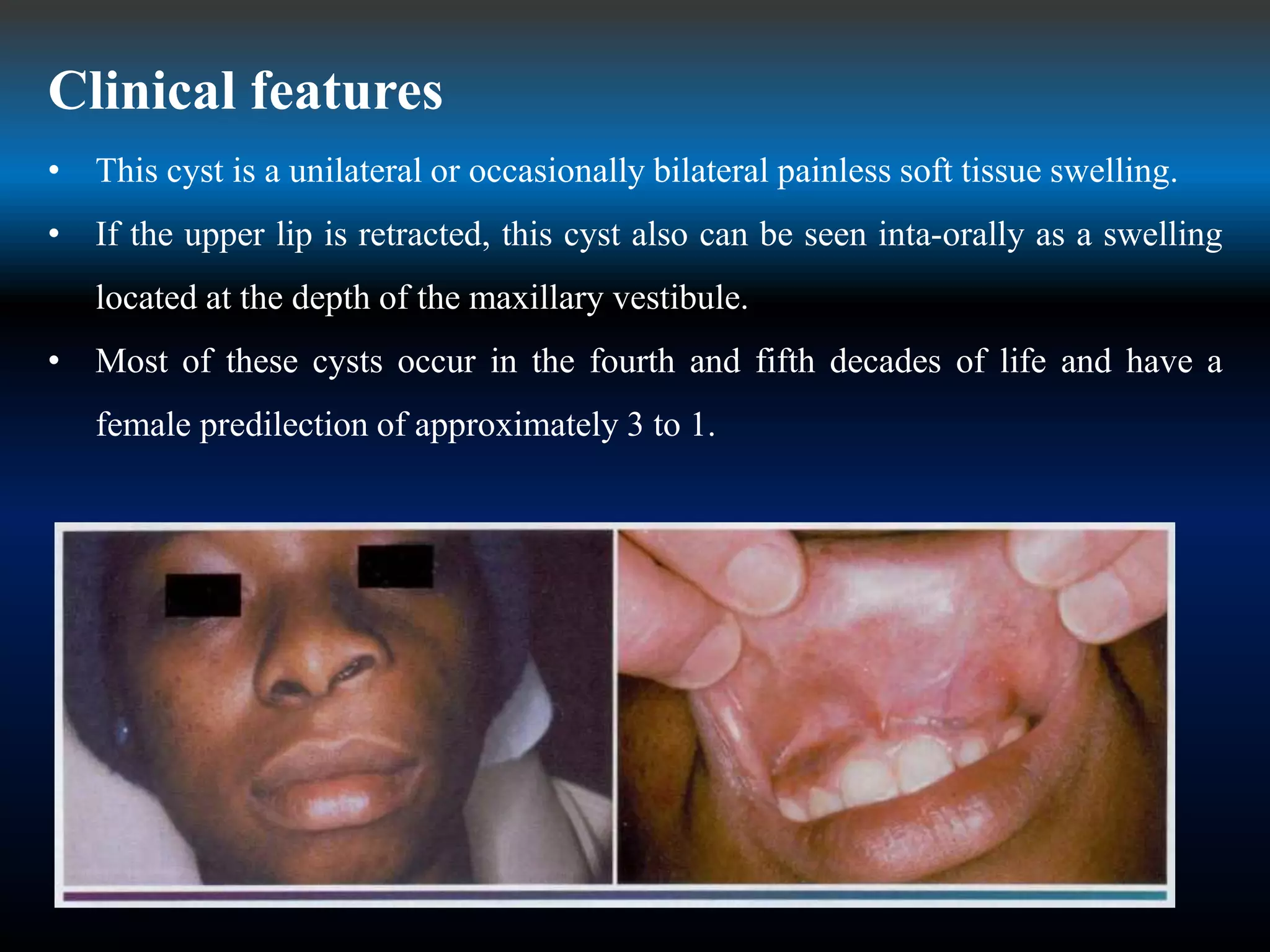
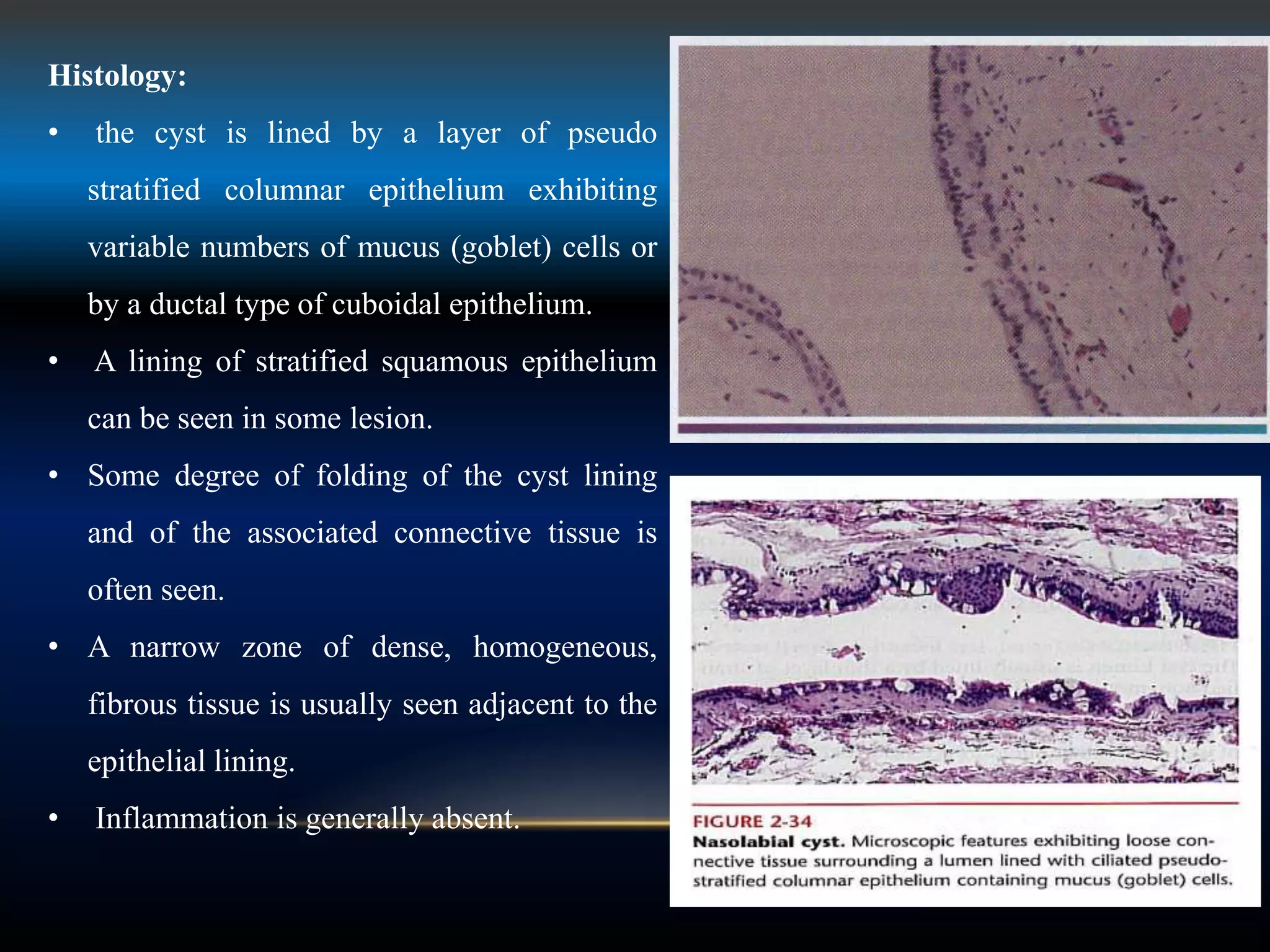
Developmental cysts can arise from epithelial remnants during embryonic development. The nasopalatine duct cyst arises from remnants of the nasopalatine duct in the midline maxilla. It appears on imaging as an oval radiolucency between central incisors. Histologically it is lined by respiratory, cuboidal, or squamous epithelium. Surgical enucleation is the treatment and recurrence is rare. The nasolabial cyst arises from remnants of the nasolacrimal duct in the soft tissues of the anterior maxilla. It presents as a unilateral swelling and is treated with surgical excision.