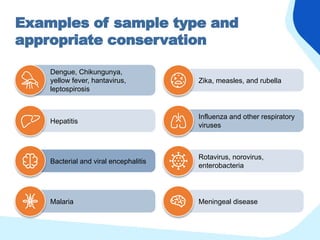
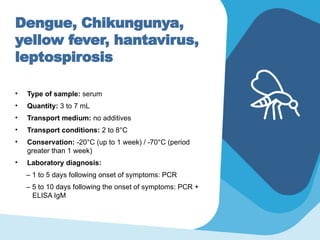
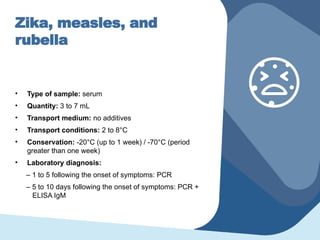
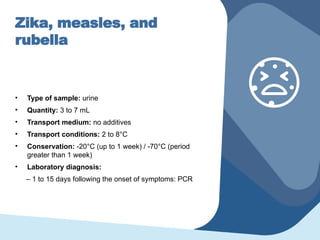
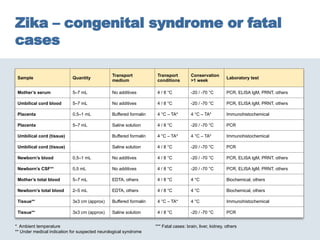
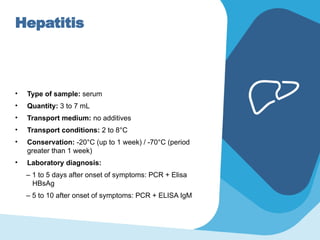
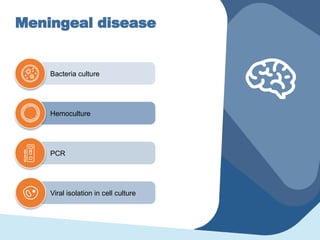
The document outlines objectives for identifying outbreak causes in work zones and discusses laboratory diagnostic methods for various syndromes prevalent in the Americas, such as febrile syndromes (dengue, chikungunya, zika), neurological syndromes, and acute diarrheic diseases. It details sample types, collection methods, conservation conditions, and laboratory diagnoses for different infections. Additionally, guidelines for specimen transport and conservation are provided for optimal laboratory diagnosis and outbreak characterization.