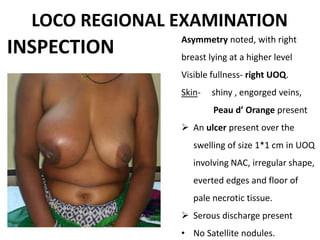
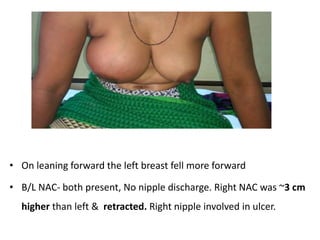
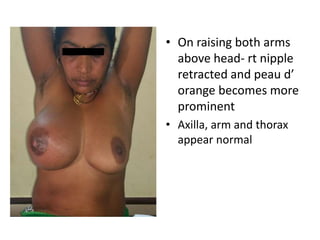
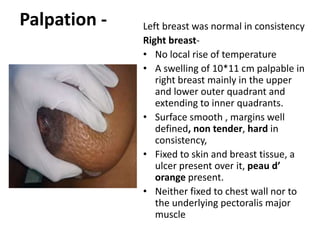
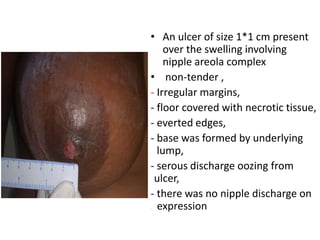
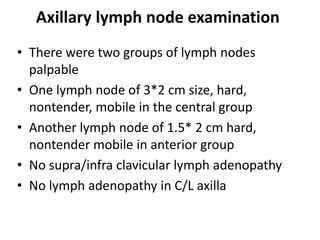
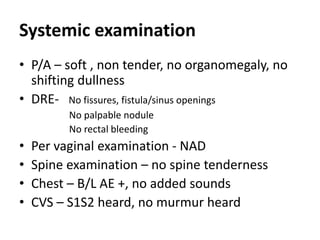
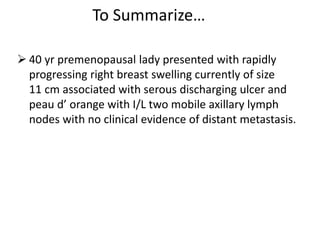
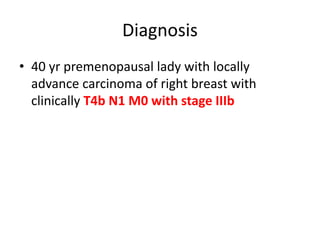
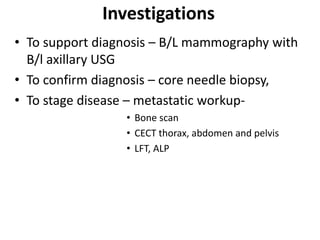
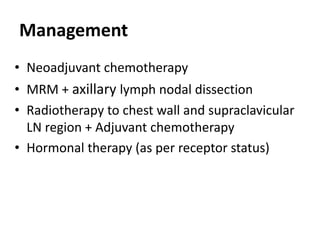
A 40-year-old Hindu lady presented with a rapidly enlarging swelling in her right breast reaching 10 cm in size over 4 months, along with an ulcerating node. Examination found a hard, fixed breast mass with peau d'orange appearance and serous discharge from the ulcer, as well as two mobile axillary lymph nodes. She was diagnosed with locally advanced carcinoma of the right breast, stage IIIb. Further tests and treatment including chemotherapy and surgery were planned.