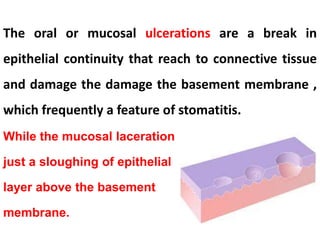
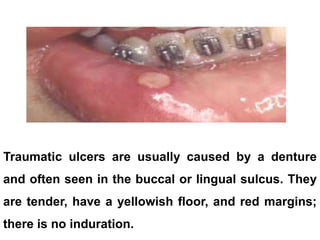
This document discusses oral ulcers and recurrent aphthous ulcers. It describes oral ulcers as breaks in the epithelial layer that damage the basement membrane, a feature of stomatitis. It then categorizes oral ulcers based on whether they involve vesiculation and if they are infective or non-infective. Recurrent aphthous ulcers are described as common, small round ulcers that typically start in childhood/teenagers and resolve by the fourth decade. Possible contributing factors include genetic predisposition, infections, immunological issues, gastrointestinal disease, nutritional deficiencies, hormones, stress and HIV infection. The document provides details on diagnosis and treatment of recurrent aphthous ulcers.