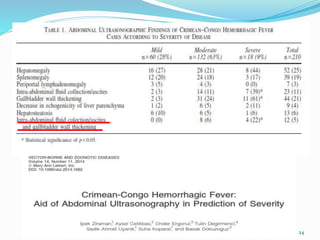
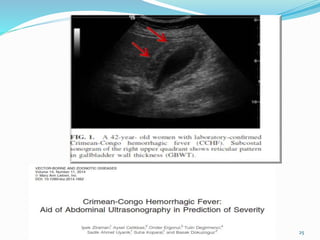
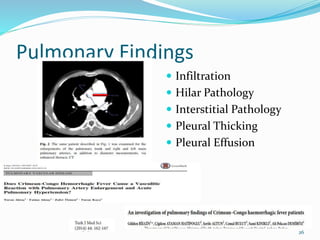
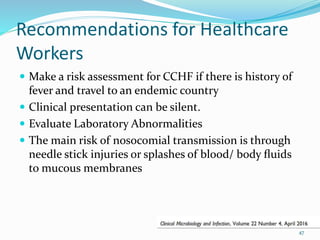
This document discusses Crimean-Congo hemorrhagic fever (CCHF), a tick-borne viral disease. It provides background on the history and identification of the CCHF virus. Key points covered include the virus classification, transmission cycle, clinical presentation, diagnosis, treatment, and recommendations for healthcare workers. CCHF presents a risk for those exposed to infected ticks or body fluids, and supportive care is the primary treatment approach.