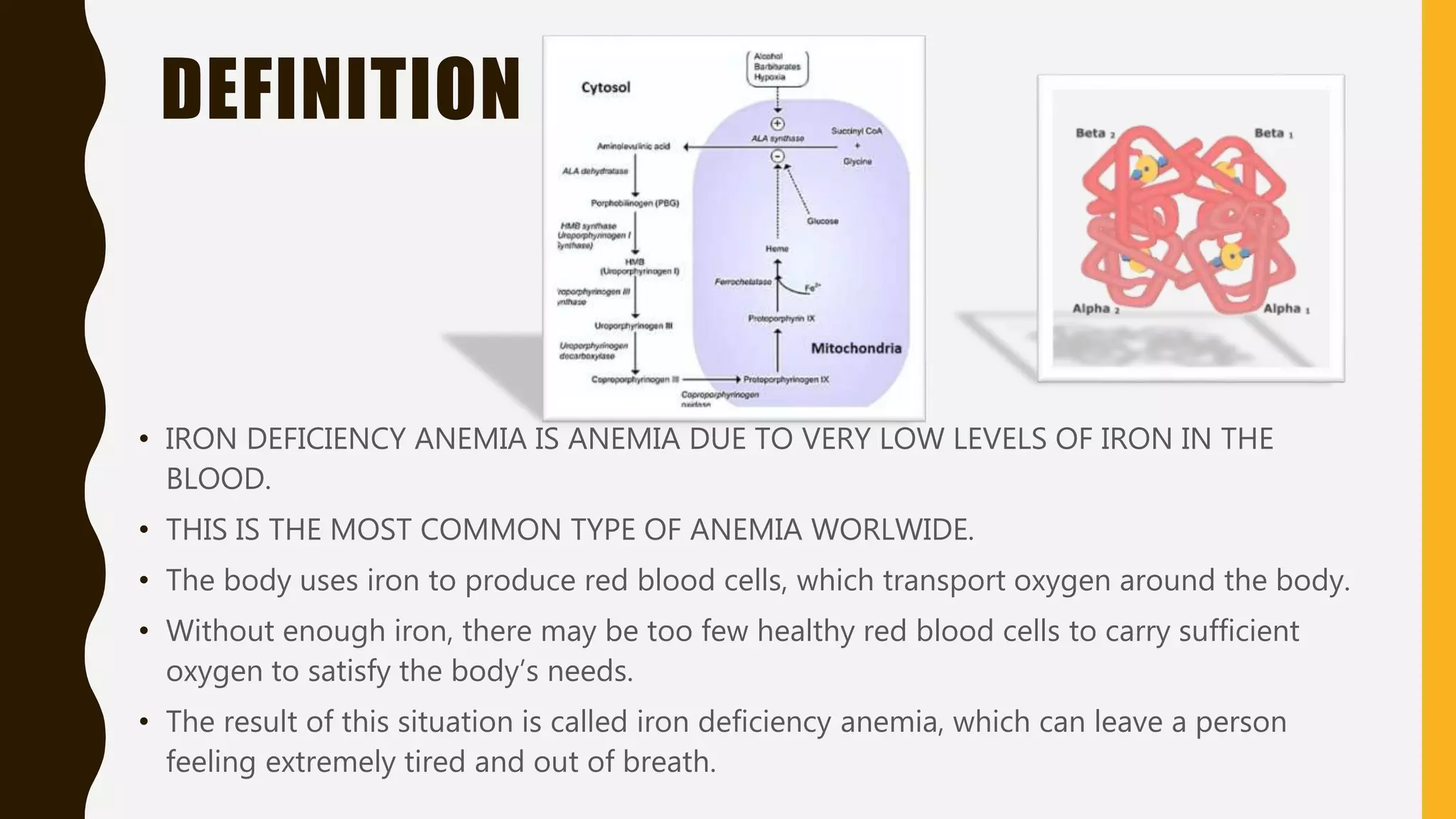
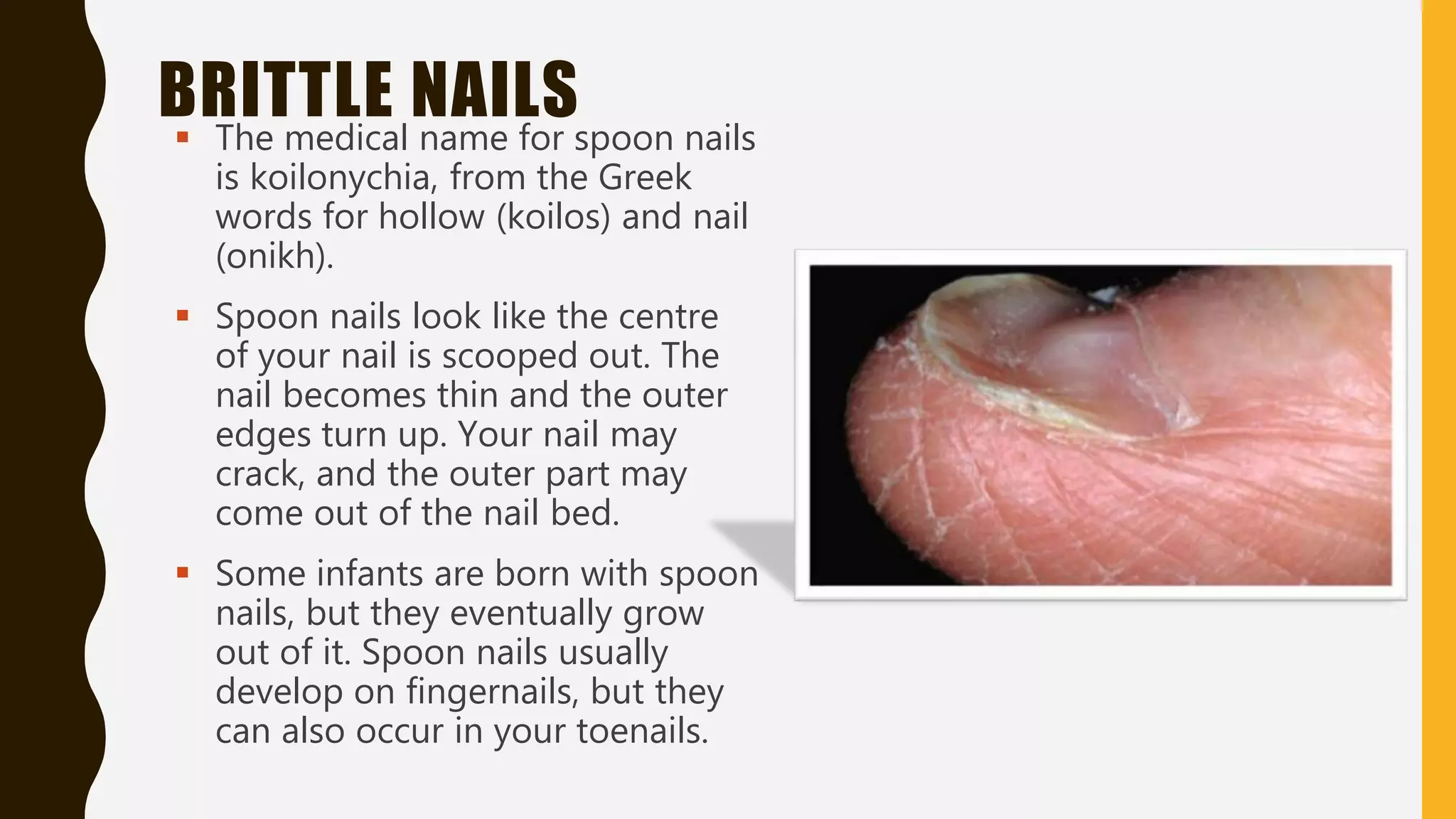
Iron deficiency anemia is caused by low iron levels in the blood. It develops in stages as iron stores are depleted. Symptoms include fatigue, dizziness, and pale skin. Those at risk include menstruating women, young children, and pregnant women. Signs of iron deficiency include brittle nails and spoon-shaped nails. Treatment involves oral or intravenous iron supplementation.